5.6 Blood Glucose Regulation
Normal Response
The monosaccharide glucose is the form of carbohydrate that is used for energy in the body. Glucose that is absorbed from the small intestine is ready for immediate use. However, fructose and galactose absorbed from the small intestine must first be converted to glucose by the liver before they can enter the bloodstream and be transported to the rest of the body to be used for energy. Once all of the monosaccharides have been converted to glucose in the liver, there are three primary uses for glucose.
- Energy. The first use for glucose is to provide energy for all the cells of the body. While all the cells of the body preferentially use glucose for energy, certain organs such as the brain and nervous system exclusively use glucose. This means that when your blood glucose levels are high, such as after eating a high carbohydrate meal, you will primarily be using glucose or carbohydrate for energy. As glucose is the fastest, most immediate source of energy, athletes and active individuals primarily rely on glucose when they are exercising at high intensities.
- Stored as glycogen. If you remember from earlier in this chapter, glycogen is the storage form of glucose in humans and animals. Excess blood glucose can be stored as glycogen in the liver and muscles. Liver glycogen can be broken down and converted back into glucose when blood glucose levels drop between meals. Muscle glycogen is “locked” in the muscle and can be broken down to glucose but that glucose can only be used by the muscle. There is a limited amount of glycogen that can be stored in the body, generally 5-7 pounds, but glycogen stores can also be influenced by diet, fitness, and exercise habits. Individuals who are more fit, generally tend to have an increased capacity for glycogen storage compared to unfit individuals (7).
- Stored as fat. If energy needs are met and glycogen stores are full, excess glucose is converted into fat and stored in adipose tissue. This is why you may have heard that “eating carbs can make you fat.” However, this situation only occurs when an individual is exceeding both their carbohydrate and calorie needs and glycogen stores are maximized. If you are an athlete or active individual, you need carbohydrates to fuel your workouts. If you wish you were more active and feel like you are always tired and do not have the energy to exercise, take a look at your calorie and carbohydrate intake. If you are severely restricting your carbohydrate and calorie intake for weight loss purposes, you may find that adding more calories and carbohydrates to your diet helps improve your energy levels so that you are able to be more active.
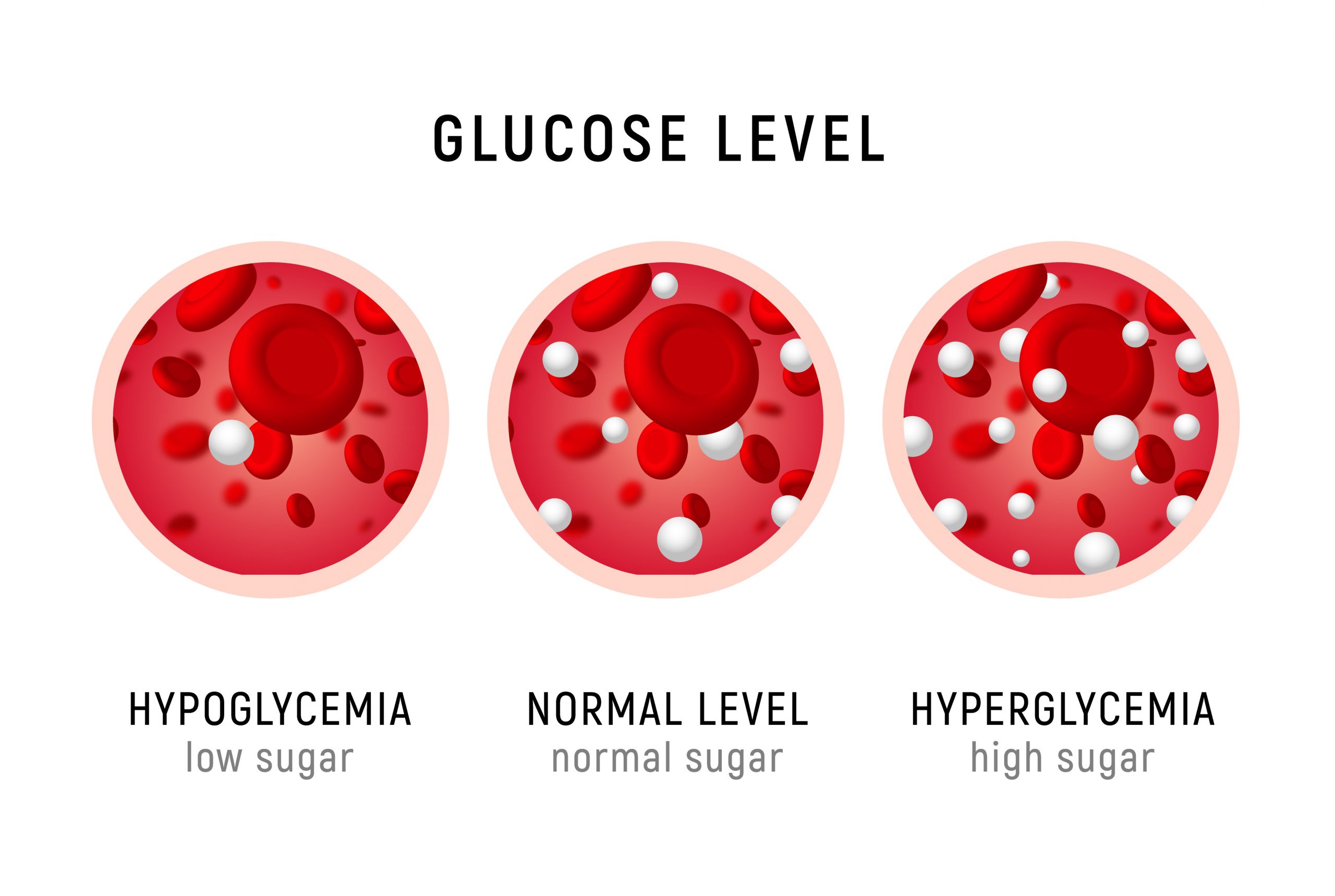
Normal blood glucose (normoglycemia) levels range between 70 and 100 mg/dl (milligrams of glucose per deciliter of blood) throughout the day. After eating a meal high in carbohydrates, blood glucose levels will rise. If blood glucose levels get too high (hyperglycemia) or too low (hypoglycemia), the body secretes hormones to bring it back into the optimal range.
Figure 5.14 Blood Glucose Levels
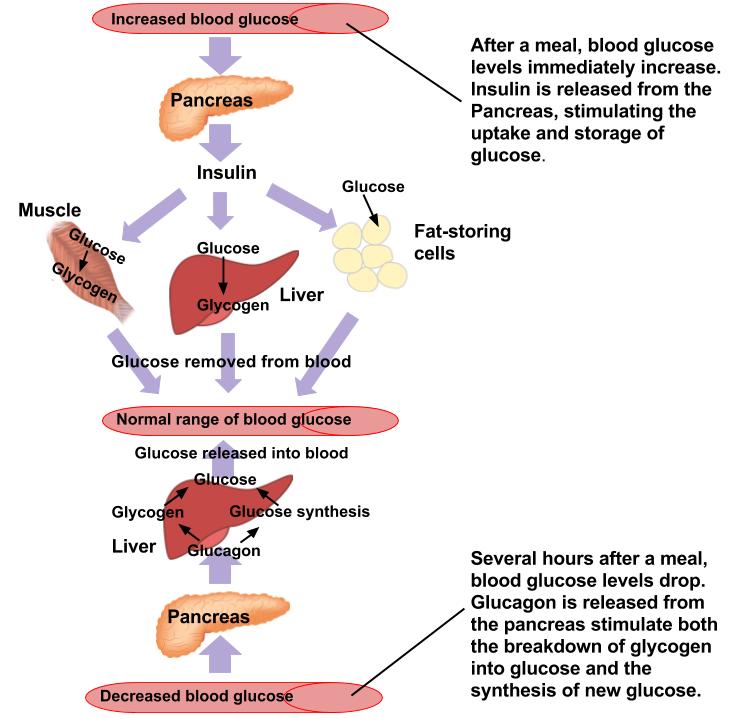
When blood glucose levels are elevated, the pancreas secretes the hormone insulin. Insulin is a hormone that stimulates the cells of the body to take in glucose from the blood therefore lowering blood glucose. The cells of muscle and adipose tissue contain glucose transport proteins, called GLUT4 transporters, to facilitate the uptake of glucose from the blood. When insulin binds to an insulin receptor, the insulin receptor is activated and signals the GLUT4 transporter to move from the interior of the cell to the cell membrane. When the GLUT4 transporter arrives at the cell membrane, it pulls glucose from the blood into the cell where it can be used for energy or stored as glycogen. Glycogenesis, or the “creation of glycogen,” is the process of storing glucose as glycogen in the liver and muscles. Therefore, insulin stimulates the process of glycogenesis in liver and muscles. Insulin does not just promote the uptake and storage of glucose, it is also the primary storage hormone for protein and fat. In addition, insulin is a satiety hormone and makes you feel full after you eat.
If the GLUT4 transporters do not arrive at the cell membrane, either because insulin was not produced or insulin does not bind to the insulin receptors, glucose will continue to build up in the blood and will not be delivered to the cells where it is needed. Independent of insulin, GLUT4 transporter’s can also be recruited to the cell membrane via muscle contraction. This is important because during moderate or high intensity exercise, the muscle cell relies on glucose as the primary source of fuel but, because insulin is a storage hormone, it is not released during exercise (8). The effects of muscle contraction on GLUT4 transporters are also a way in which exercise can help in the management of type 2 diabetes.
When you have not eaten for a period of time, blood glucose levels decrease. When this occurs, the pancreas produces the hormone glucagon. Glucagon acts on liver cells and stimulates a process called glycogenolysis, which is the conversion or breakdown of glycogen back into glucose. Glucagon stimulates glycogenolysis in the liver only because the role of glucagon is to increase blood glucose and glycogen stored in the liver can be released to the blood while muscle glycogen can only be used in the muscles. Glucagon is the primary hormone that regulates blood glucose levels between meals but because there is a limited supply of liver glycogen, liver glycogen is generally depleted within approximately 8 hours. However, this can vary dramatically depending on an individual’s initial glycogen stores. Those who chronically under consume carbohydrate will likely have depleted liver glycogen stores much sooner. Remember that the brain does not store its own glucose so it is critical that blood glucose remain in the normal range even after liver glycogen is depleted. During prolonged or overnight fasts, glucagon stimulates a process called gluconeogenesis. Gluconeogenesis means the “creation of new glucose” and takes place in the liver. During gluconeogenesis, the liver produces glucose from non-carbohydrate substances, such as amino acids from muscle tissue. Gluconeogenesis is a normal process and helps maintain blood glucose levels during prolonged periods without eating. However, if an individual chronically under consumes carbohydrate, they may struggle to maintain muscle mass because amino acids from the muscle are likely being converted to glucose to maintain brain function. Therefore, we can say that carbohydrate is protein sparing.
Figure 5.15 shows how blood sugar is regulated using insulin and glucagon.
Figure 5.15 Hormonal Regulation of Glucose
Stress Response
Insulin and glucagon are the hormones that work together to keep your blood glucose levels in the proper range during normal situations. Insulin lowers blood glucose and glucagon raises blood glucose. During times of stress, the hormones epinephrine and cortisol are released from the adrenal glands. Their main action, in relation to blood glucose, is to raise blood glucose levels, so that the muscles have plenty of glucose available for quick energy production. Epinephrine, the fight or flight hormone, provides glucose quickly by promoting glycogenolysis in both liver and muscle cells. Liver glycogen is used to raise blood glucose but muscle glycogen is broken down to glucose that remains within the muscle cells so the muscle can use it for immediate energy. Cortisol works a bit differently and is the long term response to stress. The primary action of cortisol is to stimulate the breakdown of amino acids from muscle for gluconeogenesis in the liver for long term increases in blood glucose. The stress response can be triggered by physical, mental, or emotional stress and is important for survival. If you are in a situation where you need to run for your life or fight for your life, you need the ability to produce glucose quickly. During bouts of particularly long or intense exercise (physical stress on the body), cortisol can help to increase blood glucose levels to allow a person to continue exercising at a high intensity for a longer time. The problem is when a person is chronically stressed they may experience consistently elevated levels of cortisol. This elevated cortisol can affect many body processes, hinder proper blood glucose regulation, and increase risk of chronic disease. This is why finding a way to manage stress is crucial for optimal health.
The table below summarizes the four major hormones involved in blood glucose regulation.
Table 5.2 Four Major Hormones that Regulate Blood Sugar
| Hormone | Action |
| Insulin | Produced by the beta cells of the pancreas; plays an essential role in carbohydrate and fat metabolism, controls blood glucose levels, and promotes the uptake of glucose into body cells; causes cells in muscle, adipose tissue, and liver to take up glucose from the blood and store it in the liver and muscle as glycogen; its effect is the opposite of glucagon; glucagon and insulin are a part of a negative-feedback system that stabilizes blood glucose levels |
| Glucagon | Released from alpha cells in the pancreas either when starving or when the body needs to generate additional energy; it stimulates glycogenolysis in the liver to increase blood glucose levels; stimulates gluconeogenesis in the liver in response to extended fast or starvation (when liver glycogen is depleted) |
| Cortisol | Released from the adrenal gland in response to stress; its main role is to increase blood glucose levels by gluconeogenesis (breaking down fats and proteins) in the liver |
| Adrenaline/epinephrine | Released from the adrenal glands in response to the activation of the sympathetic nervous system; increases heart rate and heart contractility, constricts blood vessels, is a bronchodilator that opens (dilates) the bronchi of the lungs to increase air volume in the lungs, and stimulates glycogenolysis in both the liver and muscles |
Media Attributions
- Blood Glucose Levels © Adobe Stock is licensed under a All Rights Reserved license
- Regulation of Glucose © Allison Calabrese is licensed under a CC BY (Attribution) license
