6.4 Cardiovascular Disease
Cardiovascular Diseases (CVD) are a group of diseases affecting the cardiovascular system. These diseases can affect the heart itself or blood vessels supplying blood to any part of the body including the heart, brain, lungs, arms, and legs. In 2019, CVD was listed as an underlying cause of nearly 900,000 deaths in the US and is responsible for more deaths than all types of cancer and lower respiratory diseases combined (1).The most common type of CVD is coronary heart disease (CHD), also known as coronary artery disease, a disease that affects the blood vessels supplying blood to the heart and is the number 1 leading cause of death for Americans.
Atherosclerosis
Atherosclerosis is a disease of the arteries characterized by hardening and narrowing of the artery wall and is the underlying process that causes most cases of CHD. However, other types of CVD can be related to atherosclerosis as well. Figure 6.15 shows the development of atherosclerosis. If atherosclerosis develops on a coronary artery (artery that supplies the heart with blood), the artery may become completely blocked and the patient will suffer a heart attack or myocardial infarction.
Figure 6.15 Stages of Atherosclerosis
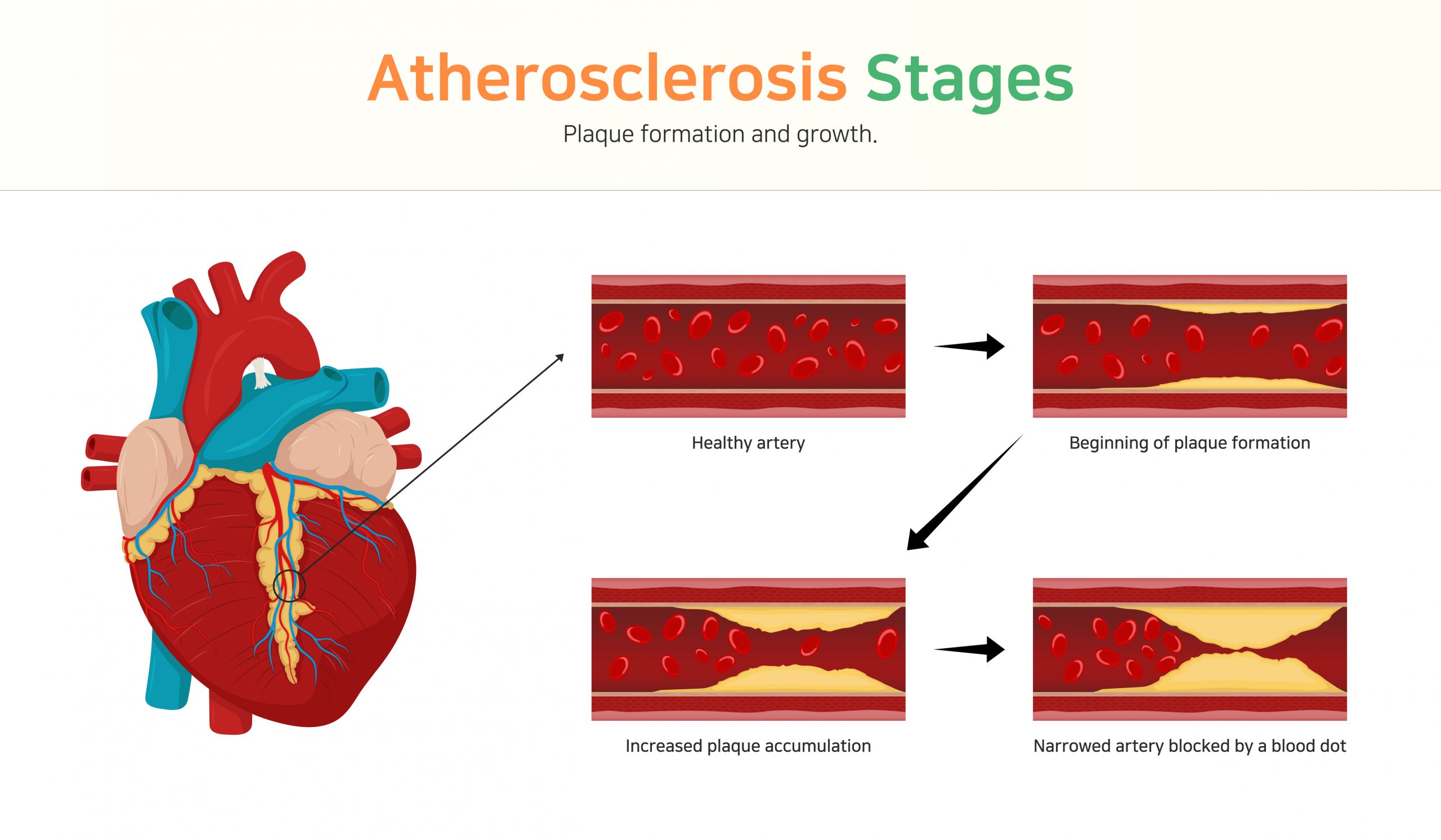
Normally, the tissues that line the artery walls are smooth and elastic and expand and contract to move blood through the arteries. Atherosclerosis causes the artery to lose its elasticity, becoming rigid and “hardened” and plaque deposits build up on the inside of the arteries. These plaque deposits are composed of cholesterol, lipid, cellular waste products, calcium, and fibrin, a protein involved in blood clotting. Over time, the plaque continues to accumulate and harden, which causes the artery to become narrower and more rigid. As atherosclerosis develops, the narrowed arteries can restrict blood supply to the heart, a condition called ischemia. In some individuals, this may result in severe chest pain called angina. Sometimes a piece of the fatty plaque breaks off and gets stuck in a smaller blood vessel in the heart, brain, lungs, or extremities.
While most individuals who die of CVD are over age 65, atherosclerosis is a chronic disease that has been shown to begin in childhood. The disease begins with an injury to the delicate inner lining of the arteries. High blood pressure, high cholesterol, smoking, stress, and other factors that increase inflammation in the body can contribute to the damage. The more of these factors that exist in an individual, the faster the disease progresses. Once the damage occurs, it leads to a very complex cascade of events that leads to atherosclerosis.
When damage occurs to the arterial lining, the body responds by initiating an inflammatory response where immune and other blood cells accumulate at the site of the injury. These cells release cytokines, which lead to the accumulation of cholesterol in the damaged artery wall from LDLs. The LDLs can become damaged or oxidized and are deposited into tears on the inner artery wall beginning the process of plaque formation. In addition to cholesterol-filled LDLs, arterial plaques contain other fatty substances, cellular debris, foam cells (macrophages [white blood cells] that engulf cholesterol), fibrin (a clotting protein) and calcium. A fragile layer of arterial tissue, called a cap, can grow over the plaques so they become embedded in the arterial wall. If the plaque ruptures, it can trigger the formation of a clot, leading to a heart attack or stroke.
Another complication from atherosclerosis is hypertension, or high blood pressure. As atherosclerosis develops, the artery loses its elasticity. Because of this, the heart has to work harder to pump blood around the body and blood pressure increases. Also, in a rigid artery, there will be more pressure against the artery wall as the blood is pumped through it as compared to a healthy flexible artery that will stretch or “give” when the blood is forced through it. The extra pressure on the artery wall causes more damage to occur which accelerates the process of atherosclerosis creating a “snowball effect” where each disease worsens the other. This is why hypertension is a major risk factor for heart failure, heart attack, and stroke. Furthermore, hypertension can cause diseased arteries to tear or rupture leading to hemorrhage and, possibly, sudden death.
Risk factors
As with all the chronic diseases that we have discussed so far, risk factors can be broken into two categories: risk factors that cannot be modified and risk factors that can be modified or changed. The more risk factors you have, the greater your chance of developing heart disease. However, even if you have one or more non-modifiable risk factors for heart disease, there are many things you can control about the process. Figure 6.16 describes strategies for reducing your risk for heart disease.
Table 6.1 Risk Factors for Heart Disease
| Non-modifiable Risk Factors | Modifiable risk factors |
| Age – risk increases with age. 80% deaths related to heart disease are in those 65 or older. | Hypertension – Having a blood pressure ≥ 140/90 increases risk |
| Biological Sex – Premenopausal women have about half the risk of having a heart attack as a man. After menopause a woman’s risk doubles and is essentially the same as a man. | High Cholesterol and Dyslipidemia – A high total cholesterol, elevated LDL, elevated triglycerides, and low HDL all increase risk |
| Family History – An individual’s risk increases if he or she has a father or brother who was diagnosed before age 55 or a mother or sister diagnosed before age 65. | Smoking – Smoking damages the walls of the arteries and accelerates atherosclerosis. |
| Race/Ethnicity – Black-Americans are more likely to suffer from heart disease than white, Hispanic, or Asian Americans. | Physical Inactivity – lack of exercise is associated with heart disease. |
| Diabetes and insulin resistance – chronically elevated blood glucose can damage the lining of the arteries. | |
| Obesity – An individual who has excess body fat, especially abdominal obesity, is at increased risk even if no other risk factors are present. | |
| Stress – Chronic stress can cause physical changes in the body that lead to arterial damage and atherosclerosis. | |
| Atherogenic diet – Dietary factors such as excessive intake of saturated fat, trans-fat, added sugar, and sodium and low intake of fiber, omega 3 fat, may elevate risk by promoting the formation of plaques. | |
| Excessive alcohol consumption – Excessive intake of alcohol can elevate risk of high-blood pressure obesity, stroke and can elevate triglycerides. |
Figure 6.16 Reducing Your Risk of Heart Disease

Metabolic Syndrome
Figure 6.17 Risk Factors that Make up Metabolic Syndrome
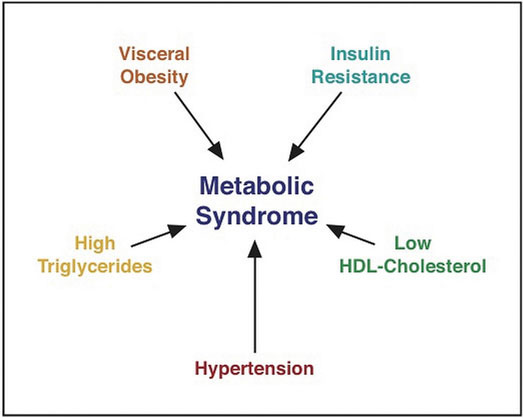
Metabolic syndrome refers to a medical condition in which people have three or more risk factors for Type 2 diabetes and cardiovascular disease (1).
- Visceral Obesity. This also is called abdominal obesity and is defined as a waist circumference >102 cm for men or >88 cm for women. Excess fat in the abdominal region is a greater risk factor for chronic disease than excess fat in other parts of the body, such as on the hips.
- High triglycerides. Blood triglyceride levels ≥150 mg/dL or taking medication to treat high triglycerides.
- Hypertension. Blood pressure ≥ 130/85 mm Hg or taking medication to treat high blood pressure.
- Low HDL-cholesterol. HDL levels < 40 mg/dL in men or < 50 mg/dL in women or taking medication to treat low HDL cholesterol.
- Insulin resistance. This is also known as elevated fasting blood sugar and is defined as fasting blood sugar ≥ 100 mg/dL or taking medication to treat elevated glucose.
Your risk for chronic diseases such as heart disease, diabetes, and stroke increases with the number of risk factors you have. A person with metabolic syndrome is more likely to develop a chronic disease than a person who does not have metabolic syndrome. The good news is that many of these risk factors can be managed with lifestyle changes such as diet and exercise. This is why it is important to know your risk factors for chronic disease. The earlier you begin taking control of your health, the less likely you are to suffer serious complications.
Hypertension
Hypertension, or high blood pressure, is a serious health problem in the United States and a major risk factor for heart disease, stroke, and kidney failure. It is estimated that nearly half of American adults suffer from hypertension. However, hypertension does not have any symptoms until blood pressure reaches very high levels, which is why it is known as “the silent killer.” The only way to find out if you have high blood pressure is to get an accurate reading of your resting blood pressure rate, which is best done by a medical professional and should be monitored regularly.
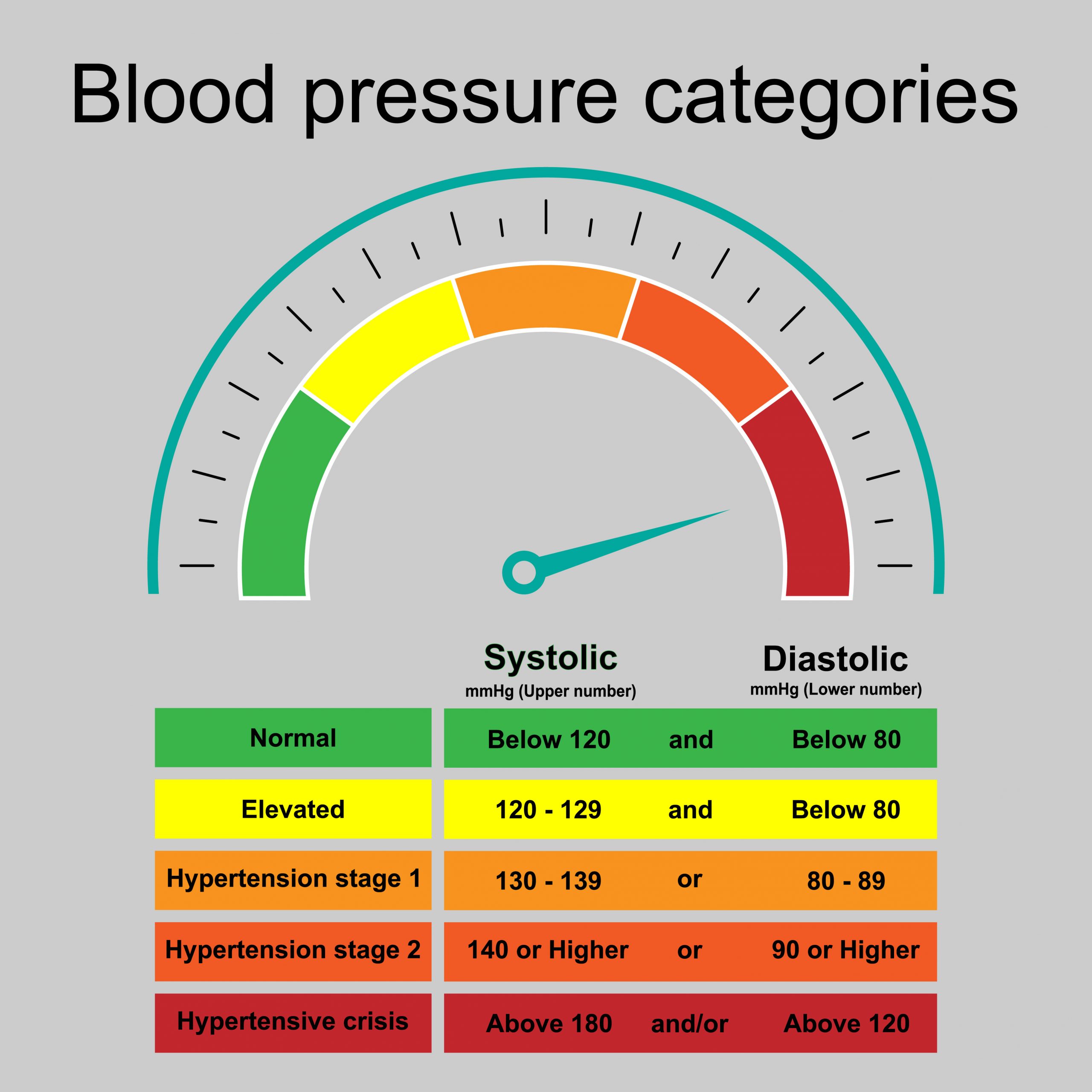
Blood pressure is the force the blood exerts against the walls of the blood vessels. When your blood pressure is measured, you will see two numbers. The top number measures systolic pressure (the pressure against the artery walls when the heart contracts) and the bottom number measures diastolic pressure (the pressure against the artery walls when the heart is relaxing and filling with blood). Blood pressure will increase in some situations when the heart is pumping more vigorously than normal such as during exercise or when a person is under stress. Therefore, in order to obtain an accurate reading, blood pressure should be measured at rest. A normal resting blood pressure is 120/80 mm Hg. Figure 6.18 lists normal blood pressure compared to various categories of hypertension.
Figure 6.18 Blood Pressure Ranges
Complications From Hypertension
As mentioned previously, hypertension is called the “silent killer” because it has no symptoms. This means that if blood pressure is not being monitored regularly an individual may not know that they have hypertension until the chronically elevated blood pressure causes enough damage to the blood vessels and organs that complications begin to appear. These complications can have signs and symptoms but by the time they are noticeable the damage has already been done.
Hypertension speeds up the development of atherosclerosis. If you have hypertension, the force exerted on your arteries is so high that it creates microscopic tears in the artery walls that then turn into scar tissue. Acting like latticework inside your arteries, this scar tissue provides a lodging place for cholesterol, platelets, and fats. This leads to plaque build up. As the plaque builds up, the arteries slowly narrow and harden, causing conditions such peripheral vascular disease, heart attack, and stroke. As you age, your arteries will naturally harden and become less elastic over time. This happens even in people without hypertension. However, uncontrolled hypertension speeds up the hardening process.
Hypertension can also cause heart failure. The narrowed arteries reduce the blood’s ability to travel through the body smoothly. This adds to the workload on the heart, making it work harder than normal. Over time, as the heart is overworked, the heart muscle bulks up and becomes larger. As the heart muscle becomes larger, the cavity inside the heart that holds blood gets smaller which means that with each contraction of the heart muscle, less blood is being pumped around the body. Now the heart has to work even harder to circulate blood and the cycle of damage to the heart continues. Eventually, the heart muscle will begin to fatigue and not be able to keep up with the body’s demands. This is called heart failure.
Hypertension can cause strokes by damaging the arteries in the brain causing atherosclerosis and creating weak places that rupture easily or thin spots that fill up with blood and balloon out from the artery wall (called an aneurysm). Approximately 10-15% of strokes in the US are hemorrhagic strokes, which occur when a blood vessel ruptures in or near the brain. When a blood vessel ruptures, it can bleed into the deep tissue in the brain or in the space between the brain and the skull. Chronic hypertension or aging blood vessels are the main causes of this type of stroke. The remaining 85-90% of strokes are ischemic strokes caused by narrowed or clogged blood vessels in the brain that cut off the blood flow to brain cells.
Hypertension can also cause kidney damage. The kidneys are the organ that filters the blood to remove toxins and waste products. This means that there are many blood vessels that pass through the kidneys. Over time, uncontrolled hypertension can cause arteries around the kidneys to narrow, weaken, or harden. These damaged arteries are not able to deliver enough blood to the kidney tissue. Also, hypertension can damage the many small blood vessels that actually filter the blood which can impact the kidneys’ ability to filter blood and regulate the fluid, hormones, acids, and salts in the body. Healthy kidneys also produce a hormone to help the body regulate its own blood pressure. Kidney damage and uncontrolled hypertension each contribute to a negative spiral. As more arteries become blocked and stop functioning, the kidneys eventually fail. This process can happen over several years, but it can be prevented by maintaining a healthy blood pressure.
Hypertension can cause erectile dysfunction. There are two root causes of erectile dysfunction: psychological and medical. Hypertension is a contributing medical factor that leads to erectile dysfunction. Hypertension damages the entire vascular system and adequate blood flow is necessary for erection.
Are you at risk?
As with all chronic diseases, there are risk factors for hypertension that can be controlled or modified and those that cannot. Table 6.2 outlines the main risk factors for hypertension.
Table 6.2 Risk Factors for Hypertension
| Non-Modifiable Risk Factors | Modifiable Risk Factors |
| Age – As age increases the risk of hypertension also increases. | Weight – Roughly 60 percent of people with hypertension are obese. |
| Race – Black Americans are more likely to develop hypertension. | Sodium consumption – Sodium intakes greater than the UL for sodium increases risk of hypertension. Most Americans consume excess sodium from salt and processed foods. |
| Family History – There is a strong genetic component to high blood pressure, and an individual’s risk goes up along with the number of family members who have hypertension. | Alcohol – Drinking more than two drinks per day for men and one drink for women increases the likelihood of hypertension. |
| Diet – In addition to salt and alcohol consumption, other dietary factors increase chances of developing hypertension. | |
| Smoking – The nicotine in cigarettes and other tobacco products acts as a stimulant that increases risk of hypertension. | |
| Stress – Chronic stress increases the likelihood of hypertension. | |
| Inactivity – Physical activity can strengthen the heart and blood vessels which allows the heart to pump blood through the body more effectively and reduce blood pressure. |
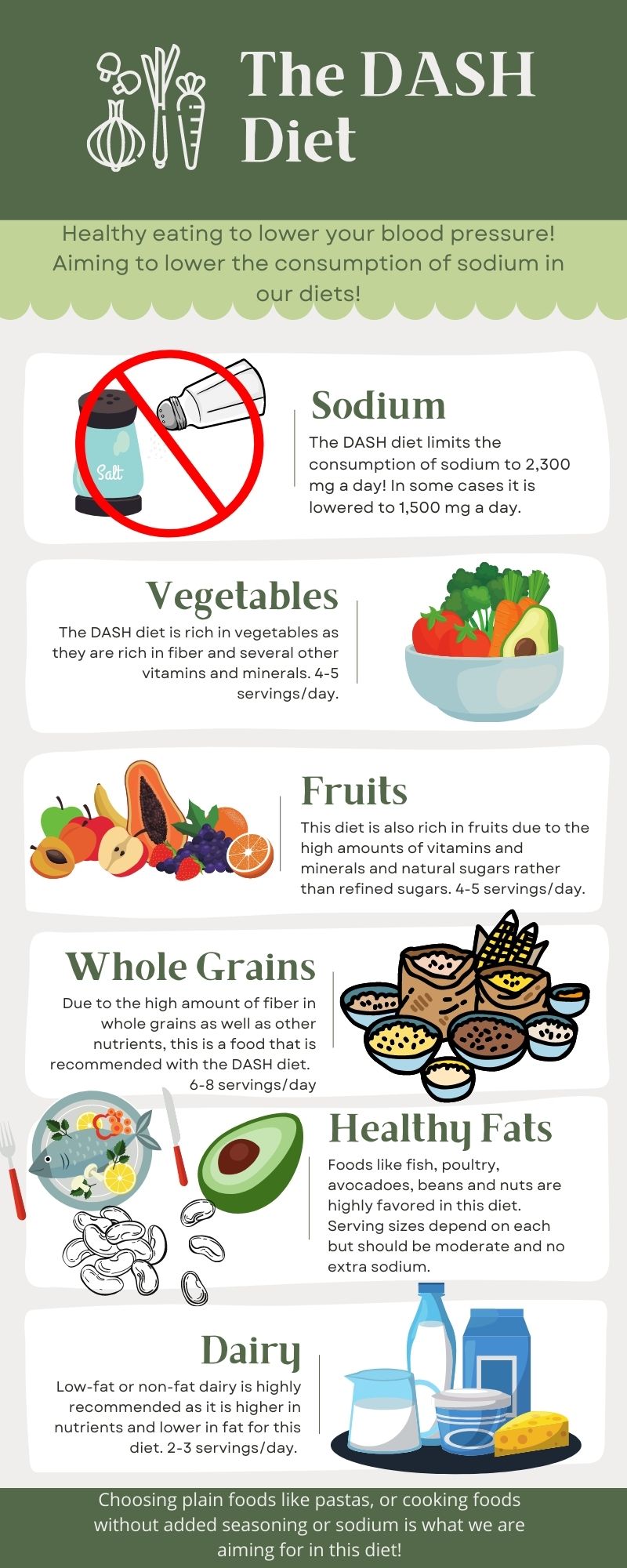
The Dietary Approaches to Stop Hypertension, or DASH diet, focuses on reducing sodium intake to either 2,300 milligrams per day (as recommended by the Dietary Guidelines for Americans) or 1,500 milligrams per day for certain populations at risk for hypertension. The DASH diet is an evidence-based eating plan that can help reduce high blood pressure (2). This plan may also decrease the risk of heart attack, stroke, diabetes, osteoporosis, and certain cancers. DASH tips to lower sodium include:
- Using spices instead of salt to add flavor
- Reading sodium content on processed or canned food labels, and choosing low-sodium options
- Removing some sodium from canned foods (such as beans) by rinsing the product before consumption
- Avoiding salt when cooking
DASH dieters are recommended to consume a variety of whole grains and high-fiber fruits and vegetables, and moderate amounts of low-fat dairy products, lean meats, and heart-healthy fish. In addition, DASH limits the use of saturated fats to less than 7 percent of total calories, and limits the consumption of sweets and alcohol. The DASH diet also calls for consuming less added sugar and drinking fewer sugar-sweetened drinks. It replaces red meat with fish and legumes and calls for increased calcium, magnesium, potassium, and fiber.
Figure 6.19 Dietary Approaches to Stop Hypertension (DASH)
Media Attributions
- Stages of Athersclerosis © Adobe Stock is licensed under a All Rights Reserved license
- Reducing Risk of Heart Disease © Natalie Fox is licensed under a CC BY (Attribution) license
- Metabolic Syndrome © University of Hawaii is licensed under a CC BY-NC-SA (Attribution NonCommercial ShareAlike) license
- Blood Pressure Ranges © Adobe Stock
- The DASH Diet © Natalie Fox is licensed under a CC BY (Attribution) license
