9.1 Obesity
Much of the dissatisfaction around weight is a result of society’s attitude toward obesity. To many, it is viewed as a social and professional handicap. Many terms have been coined that reflect society’s prejudice against overweight and obese individuals; fat bashing, fattism, fat shaming. As a result, we are obsessed with losing weight and we spend a lot of money to do so. Despite all the money spent, obesity rates have increased dramatically in the United States over the last several decades.
In 1962 about 46% of adults in the United States were considered overweight, obese, or extremely obese. About 32% of adults were overweight, about 13% were obese, and about 1% had extreme obesity. Percentages of adults within all of these categories increased gradually until the late 1970s, at which point they began to climb more quickly, leveling off somewhat around 2000. The increase was most dramatic within the obesity category, while the percentage of overweight adults held fairly steady, and the percentage of adults with extreme obesity increased moderately.
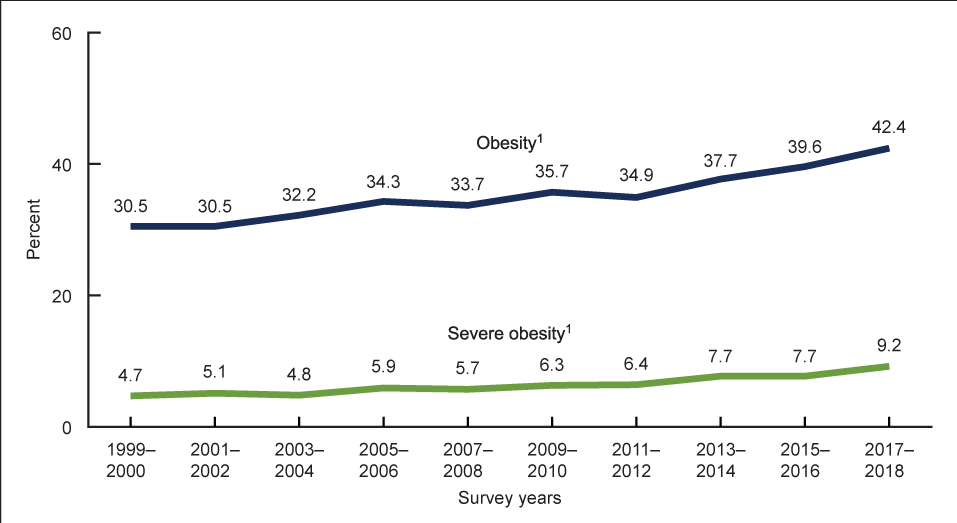
Around 2000, about 70% of adults were considered overweight, obese, or extremely obese. Of this group, 34% were considered overweight, about 31% were considered obese, and about 5% were considered to have extreme obesity. By 2018, about 42% were considered obese, and about 10% were considered extremely obese (2). Overweight and obesity are also increasing rapidly in children. Childhood obesity has more than doubled in children and quadrupled in adolescents in the past 30 years.
Figure 9.1 Trends in Obesity and Severe Obesity Among American Adults
Obesity rates are also higher among certain groups of people. Rates of obesity are higher among those living in the states of the Deep South and Midwest and vary by racial group with 49.6% of non-Hispanic Black, 44.8% of Hispanic, 42.2% of non-Hispanic White, and 17.4% of non-Hispanic Asian adults considered obese. Socioeconomic status is also associated with obesity and those with college degrees and higher incomes are less likely to be obese (2).
Obesity is not just a problem in the United States; it is becoming a worldwide epidemic with obesity rates tripling between 1975 and 2016 (3). Obesity rates have skyrocketed in westernizing countries and in the urban areas of developing countries. Paradoxically coexisting with undernutrition, an escalating global epidemic of overweight and obesity—“globesity”—is taking over many parts of the world. Throughout the world, overweight and obesity are responsible for more deaths than underweight. Many low- and middle-income countries are now facing a “double burden” of disease. While they continue to deal with the problems of infectious disease and under-nutrition, they are experiencing a rapid upsurge in noncommunicable disease risk factors, such as obesity and overweight, particularly in urban settings. It is not uncommon to find under-nutrition and obesity existing side-by-side within the same country, the same community and the same household.
Why Is Excess Body Fat Unhealthy?
So how do we define “overweight” and “obese”? Overweight and obese refer to a body weight that is higher than what is considered healthy for a given height. Obesity can be further distinguished by the fact that it generally involves excessive and unhealthy amounts of body fat that are likely to result in obesity-related illnesses or disorders. It is important to note that being overweight is generally not unhealthy unless the extra weight is from excess body fat. In this chapter, the term overweight will be used to describe people who have too much body fat but are not obese. So then, what is a healthy weight? A healthy weight is one that does not increase your risk of developing weight-related health problems. Generally, a healthy weight is expressed as a range of weight that is appropriate for your age, sex, height, and muscle mass. A healthy weight range should be realistic and sustainable and allow you to feel healthy, energized, and fit.
There are negative health effects at both ends of the weight spectrum; being underweight can result in compromised immune function, nutritional deficiency, electrolyte imbalances, and low energy levels. Over time, more serious health complications can arise. Overweight and obesity are related to several different disorders and chronic diseases. Generally, as a person’s weight increases the number and severity of health problems increases. For example, a person may develop borderline hypertension as they become overweight. As they accumulate more body fat, the hypertension worsens and they develop insulin resistance as well, eventually contracting type 2 diabetes.
What Causes Obesity?
Obesity is caused by a complex interaction between genetics, environment, and lifestyle. There is no single cause of obesity but there are many things that can contribute. Overweight and obesity result from an energy imbalance. The body needs a certain amount of energy from food to keep up basic life functions. Body weight tends to remain the same when the number of calories eaten equals the number of calories the body uses or “burns.” Over time, when people eat and drink more calories than they burn, the energy balance tips toward weight gain, overweight, and obesity. Many factors can contribute to energy imbalances and weight gain. As stated earlier, factors such as genetics, eating habits, how and where people live, life habits, education, and income can all interact to cause weight gain and obesity. Because of the complexity, obesity is difficult to reverse, so we must focus on prevention to reverse this health epidemic.
Genetics has a strong influence on body weight and deserves a more in depth look. If your mother or father is overweight, your risk of becoming obese doubles, if they are obese your risk triples, and if they are severely obese it increases fivefold. Research also suggests that people who are genetically predisposed to being overweight have a more difficult time preventing obesity when exposed to a food environment that is conducive to weight gain. An easy way to understand this concept is with the analogy that “genetics loads the gun, but lifestyle pulls the trigger.” A person with a genetic predisposition to obesity will always have a more difficult time maintaining a healthy weight. However, when they are exposed to an environment where they have easy access to a myriad of cheap, calorie-dense, unhealthy foods, maintaining a healthy weight becomes almost impossible. This is referred to as a gene–environment interaction. However, genetic predisposition is not genetic destiny. If you make healthy dietary choices and live a healthy lifestyle, it will be easier to maintain a healthy body weight, even if you are predisposed to obesity and other diseases.
When it comes to an individual’s environment, there are many things that cause us to be more sedentary and to eat more than we should. Jobs that require us to sit for long periods of time, less time for food shopping, preparation and cooking, eating out more, and just eating too much. Food is everywhere, at the bookstore, the coffee shop, vending machines in the workplace, and on every street corner. It is almost impossible to avoid! When it comes to weight gain, technology has been our worst enemy. We can communicate with people around the globe without leaving our beds. We can work and attend classes remotely without getting dressed and commuting. Since our work can all be completed on our devices we don’t need to move from classroom to classroom or physically walk across the office to communicate with others. While there are many benefits to this connected world, there is no doubt that this technology increases our sedentary behavior. Research has shown that the COVID-19 pandemic led to a decrease in physical activity and increase in sedentary behavior among both children and adults (4). This increased sedentary time increases our risk of gaining weight and developing health problems. Even outside of work technology has reduced our calorie burning. We use a dishwasher instead of washing dishes by hand, we drive short distances rather than walk or ride a bike, and we now pay someone to clean our homes rather than do it ourselves. All of these things that make our lives easier have made our health worse. More than half of Americans do not even meet the recommended 30 min/day of moderate intensity physical activity. The bottom line is; in the past three decades we have been moving less and eating more. If we want to reverse the obesity trend in this country, we need to move more and eat less (and healthier)!
Many people become obese as they age, in fact, it is become so common that many people believe it is inevitable. This is referred to as creeping obesity because it “creeps up” on adults slowly over time. Most people will gain some weight as they get older and in some cases it is beneficial, but adult onset obesity is not normal nor is it unavoidable. Excessively lean older adults are more likely to suffer from osteoporosis and fractures and, in the event they do get ill, they often do not recover as well due to low energy stores. However, in older persons, obesity can exacerbate the age-related decline in physical function and lead to frailty. Weight gain in adulthood is mainly a result of becoming more sedentary as we age without adjusting our energy intake downward to compensate for a lower energy expenditure. In other words, we eat the same amount but do less. In addition, the loss of muscle mass that accompanies a sedentary lifestyle further reduces calories burning, compounding the problem. Even if you do maintain an active lifestyle and participate in muscle building activities, the hard truth is that you still may need to eat less calories due to the natural effects of aging.
Can You Be Overweight and Healthy?
There is an overwhelming assumption in our country that if an individual is overweight they are also unhealthy. Research clearly supports that being overweight is a major health risk factor for chronic disease. So does this mean that if you are carrying around some extra pounds that you are destined to be unhealthy? Some of the current research on the topic has found that the answer to this question is “no.” And that we should be more focused on monitoring our health, and less focused on monitoring our weight. The first major study to look at this was conducted by researchers at the Cooper Institute, a nonprofit organization in Dallas that promotes fitness. In an observational study of 22,000 men, ages 30–83, the researchers measured subjects’ body composition and assessed their cardiovascular fitness status using treadmill tests. During eight years of follow-up, 428 of the men died. Men who were overweight but fit (as measured by a treadmill test) were two times less likely to have died than men who were lean but not fit. Moreover, the all-cause mortality rate of fit, overweight men was not significantly different from that of the fit, lean men (5). In another observational study using the same protocol in women, it was discovered that cardiovascular fitness was a better predictor of mortality than BMI and 50% of women who were categorized as overweight or obese based on their BMI had high levels of cardiovascular fitness (6). This shows that not all individuals with high BMIs have low cardiovascular fitness. The conclusion: If you are fit, being overweight does not increase mortality risk. Another came to a similar conclusion. For almost four years, the researchers tracked heart attacks and other “cardiovascular events” among 900 American women. They found that lack of physical activity was a better predictor of an adverse event than weight (7). Current research suggests that a weight neutral approach to health may be better than focusing on “losing weight” and interventions to improve health should focus on sustainable ways to increase physical activity without obsessively monitoring weight (8). This may help many adults get out of the spiral of trying to lose weight in unhealthy manners and then gaining the weight and more back. In conclusion, regular exercise has health-promoting effects, which are beyond its effect on weight control. Apart from any weight-loss goals you have set for yourself, it is important to exercise regularly and monitor health parameters, such as cholesterol, blood pressure, and glucose.
Media Attributions
- Obesity Trends © CDC is licensed under a Public Domain license
