1
Overview of the U.S. Healthcare System
Whitney Hamilton, DrPH
Middle Georgia State University
Thomas A. Clobes, PhD
California State University, Channel Islands
“Every single one of us deserves access to quality, affordable health care.” – Sara Gideon
Learning Objectives
- Discuss the key principles of the healthcare system in the United States
- Outline the basic structure of the U.S. healthcare system
- Explain the advancement of the U.S. healthcare system over time
- Discuss the tri-fold challenges of rising healthcare costs, unequal access to quality care, and negative health outcomes in the U.S.
- Emphasize a shift in the traditional nature of the U.S. healthcare system to a system of value-based care
Introduction
The U.S. healthcare system is facing dynamic and ever-changing operating and financial environments due to steeply rising medical costs, heavy patient demands, and complex regulatory compliance standards. As a result, the current healthcare industry is deeply fragmented, costly, inequitable, and uncoordinated. This chapter will outline the major components of the system, highlight the major factors impacting the healthcare industry’s operating and economic environment, and provide a historical overview of the U.S. healthcare system.
Key Components of the U.S. Healthcare System
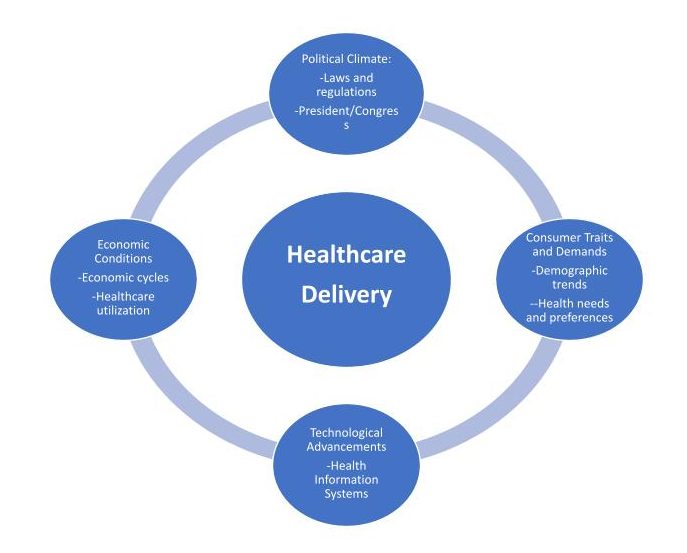
A fully functional healthcare system operates based on the needs and expectations of its consumers and is systematically structured to improve the overall health of the population. The healthcare system should be designed to protect the public from outbreaks, to provide equitable access to healthcare, and to enable patient engagement while reducing the burden of costly medical care (World Health Organization, 2010). The healthcare system is subject to external forces, such as the political climate, shifting demands and preferences of the consumer, technological advancements, and financial constrictions, that have a direct impact on its structure. The effect of these forces influences the delivery of healthcare, including the access, equitability, cost, and quality of healthcare. The U.S. healthcare system provides some of the best medical care in the world, but neglects to consistently deliver equitable and affordable services to the most vulnerable populations due to the impact of these external forces.
External Forces Affecting the Delivery of Healthcare![]()
The U.S. healthcare system is not a fully coordinated system. In fact, it is difficult to characterize U.S. healthcare as a system at all. The Merriam-Webster’s dictionary definition of a system is “a regularly interacting or interdependent group of items forming a unified whole.” The healthcare system in the United States is made up of loosely structured insurance, delivery, payment, and financing networks. There are five key stakeholders that make up the U.S. healthcare system: the healthcare consumers, the insurers and payers, the healthcare providers, medical suppliers, and the policy-makers and regulators.
Healthcare Consumers
Healthcare consumers are the individuals who are the recipients of healthcare services (Institute of Medicine, 2010). They may also be referred to as patients. Although consumers play a major role in healthcare decision-making, consumers typically depend on the advice of healthcare professionals for medical decisions, but may be unaware of the underlying financial obligations. For example, a patient may elect to undergo a medical procedure with an in-network provider, a provider who has negotiated rates with the insurance company to provide specific services at a designated rate (Institute of Medicine, 2010). However, unbeknownst to the consumer, the provider may have an out-of-network staff, for instance, an anesthesiologist, that charges full prices for the services provided, leaving the consumer with an expensive, out-of-pocket bill. It is important the consumer is completely aware of their medical decisions and inquire about fully in-network providers and options.
Healthcare Spending and Financing: The Insurers and Payers
Healthcare financing depends on the collection of money for healthcare services and the reimbursement of health providers for the rendered services. The payers include private sector (insurance companies), the public sector (government and state agencies), and the consumers (out-of-pocket expenses) that share responsibility for the financing functions (NCSL, 2020). The third-party payer is any organization that pays or insures healthcare expenses for the healthcare consumer. Each service provided to a consumer has a designated fee attached called a charge (set by the provider) or a rate (set by a third-party payer). Healthcare providers often rely on the patients’ insurance to obtain payment for rendered services. This controls how much the provider is paid for his/her services. Financing makes access to healthcare easier, thereby increasing the demand for healthcare services. The United States is a multi-payer financing system. Unlike most developed countries that have a single payer system, where national health insurance programs are run by the government and financed through taxes, the U.S. healthcare system is comprised of a complicated mix of public and private, for profit and non-profit insurance and providers (Donnelly et al., 2019).
Although the U.S. government finances healthcare through government and state programs for certain groups of people, such as the elderly, low-income, children, and veterans, who meet the program’s proposed eligibility requirements, the U.S. does not provide overall healthcare to all of its citizens leaving approximately 30 million individuals, equating to nearly 9.2% of the U.S. population, uninsured as of 2019 (Rosso, 2021).
Medicare is a public health insurance provided by the federal government to persons aged 65 and older or individuals under 65 with permanent disabilities (Medicare, 2022; Rosso, 2021; Tikkanen et al., 2022). Under the traditional, fee-for-service Medicare plan, the government directly pays for the healthcare services received by the beneficiary. The beneficiary will typically pay a co-insurance (or, a co-pay, which is not synonymous with co-insurance; for more information, please refer to Chapter 9 on Managed Care) for each service received, which is a required payment that the beneficiary is responsible for after the insurance pays a fixed amount (Medicare, 2022). Medicare has four main parts that cover specific services. Part A provides coverage for in-patient/hospital services and part B provides outpatient/medical coverage. Part C, also known as the Medicare Advantage Plan, offers an alternate plan to the traditional, fee-for-service Medicare plan. Both the traditional, fee-for-service and Medicare private plan require beneficiaries to pay a monthly premium; however, the Medicare Advantage Plan has different requirements, rates, and restrictions on how and when care can be received. The final part of Medicare, Part D, provides coverage for prescription drugs (Medicare, 2022; Tikkanen et al., 2022;).
Another public, health insurance plan is Medicaid, which is a state-administered health insurance program that provides health care services to low-income families as well as individuals with disabilities (Rosso, 2021; Tikkanen et al., 2022). The eligibility requirements differ by state as it is a state-administered program. The Children’s Health Insurance Program (CHIP) is another state-administered program for low-income children whose families’ earnings disqualify them for Medicaid but still the earnings are inadequate enough to afford private insurance (Rosso, 2021; Tikkanen et al., 2022).
TRICARE is a healthcare program for military personnel and their families provided by the Department of Defense. TRICARE functions as a government-managed health insurance and is divided into various types of coverage programs for active-duty, reservists, and retired military personnel and their families. In 2019, approximately nine million individuals had TRICARE insurance (Rosso, 2021).
While the United States does pay for healthcare for specific groups the government and state-administered health programs, the financing and insurance functions of healthcare delivery remains a largely market-oriented, privatized entity. Any health insurance coverage that is not offered by the state or federal government is considered private health insurance. The majority of health insurance plans are private and provided by employers. Although most individuals in the United States are insured by their employer or the government, individual health insurance is available for people who are self-employed or unable to access an employer or government health plan. In many states, employers are not required to provide its employees with health insurance (Rosso, 2021). Further, some small businesses are unable to provide health insurance benefits because they cannot obtain affordable health insurance group rates, leaving many employed individuals without health insurance. Employed individuals earning low-incomes are the most likely to be uninsured because they cannot afford the premium cost sharing and are ineligible for government benefits. Typically, individual insurance plan rates are higher than the employer’s group rates.
The individual health insurance markets comprise of plans purchased directly from the insurer. These private insurance entities, the group (employer-sponsored) and non-group (individual market), typically seek to control healthcare financing for corporate gain, without consideration for the impact to the entire healthcare system. Health insurance companies are unable to operate at a loss, they have to receive more money in premiums than they pay out for medical claims (Rosso, 2021). The interests of the different payers are often at odds. For instance, healthcare providers may seek to increase the reimbursement for services rendered to Medicaid beneficiaries, while the government aims to restrict cost increases. Employers may also seek to contain increases to health insurance premiums and the health plans, as a result of disgruntled employers, may constrain healthcare providers fees, who resent the reimbursement cuts. The various players in the healthcare system create a conflicting environment that makes cost containment and system-wide reform difficult (National Academy of Engineering & Institute of Medicine, 2005).
However, the Affordable Care Act (ACA) was initiated in 2010 in an attempt to reform the U.S. healthcare system and provide an expansion of health insurance to cover the large number of uninsured individuals. The ACA requires that all U.S. citizens and legal residents be covered by public or private insurance, and failure to do so will require the uninsured to pay a tax, with some exemptions, such as religious beliefs and financial hardships. However, the Trump Administration removed the individual mandate, and as of 2019, the tax penalty has been repealed. The ACA also requires insurance plans to cover young adults under their parents’ policies until they are 26 years of age (NCSL, 2011). There are three key tenets of the ACA:
- Enables states to expand Medicaid coverage to individuals with incomes 138% below the federal poverty level
-
Establishes state-based insurance marketplaces to keep prices competitively lowEmphasizes prevention and wellness efforts
Between the years 2010 and 2021, the number of uninsured in the United States greatly declined from 48.2 million to 30 million individuals. Although the Affordable Care Act has made significant progress increasing the accessibility and affordability of healthcare, many Americans are still left without health insurance (Finegold et al., 2021; Rosso, 2021). Policy makers must find a way to shift to a single payer system or find a way to use the United States’ distinctive multi-payer financing to improve the population’s overall health and reduce healthcare inequalities. The U.S. healthcare system must develop stronger regulations and compliance standards regarding healthcare costs and coverage (WHO, 2010).
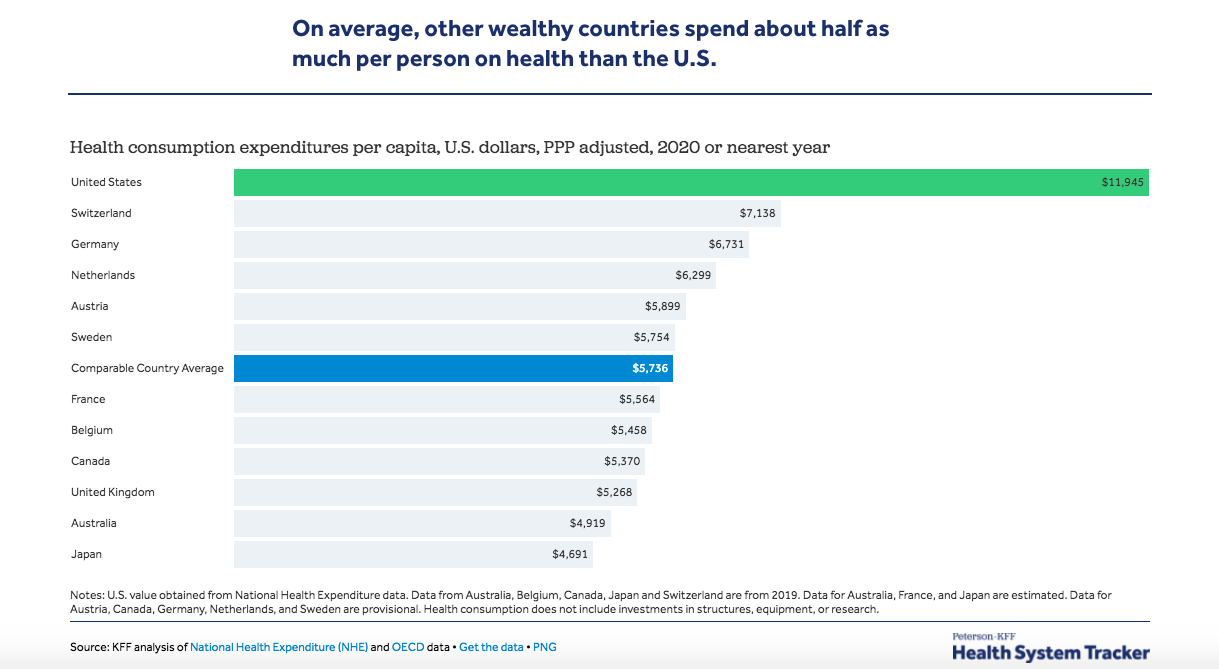
The United States spends more per capita on healthcare than any other comparable high-income country and continues to spend more on healthcare at an unsustainable rate (OECD, 2019; PWC Health Research Institute, 2019). In 2019, nearly 3.6 trillion dollars were spent by uninsured individuals, private health insurers, federal and state governments, on health consumption expenditures accounting for approximately 17% of the nation’s gross domestic product (GDP) (Centers for Medicare & Medicaid Services, 2019; Wager et al., 2022). Following the COVID-19 pandemic, the U.S. spent nearly 10% more on healthcare, totaling more than 19% of its GDP on healthcare (Wager et al., 2022; Centers for Medicare & Medicaid Services, 2019). The GDP is the total monetary or market value of all the finished products and services that are produced within a country during a specified time frame. In other words, the GDP provides a scorecard of a country’s economic health.
Healthcare spending is closely tied to a country’s wealth; however, comparing health expenditures across countries can be complicated due to unique health system structuring, political, and economic features that affect each country’s spending (Wager et al., 2022). However, the Organization for Economic Cooperation and Development (OECD) consists of 38 countries with above median national and per person incomes that commit to democratic and market principles enabling comparisons to be drawn on the political and economic experiences between the high-income nations (Wager et al., 2022). As previously mentioned, the United States spends more on healthcare, than all other countries in the OECD while some countries, such as Turkey, spends as little as 4% of their GDP on healthcare. In 2020, the U.S. spent $11,945 on health expenditures per person, which was nearly twice as much as the average $5,736 the other high-income OECD countries spent on health per person. Although health spending increased between 2019 and 2020 for all of the developed nations following the global pandemic, the U.S. was already spending the most per capita on health (Wager et al., 2022).
Healthcare Providers
Healthcare providers include all of the individuals and organizations that provide healthcare services to a consumer. Healthcare practitioners, group medical practices, hospitals, nursing homes, and ambulatory facilities (rehabilitation, surgery, imaging etc.) are examples of healthcare providers. Please see chapter 2 for an overview of healthcare providers.
Healthcare Suppliers
The healthcare suppliers are the companies including the pharmaceutical and medical equipment companies that supply and distribute medical supplies and medicine. Healthcare suppliers play a major role in the healthcare system by providing medical supplies, such as wheelchairs, C-PAP machines, oxygen and medication that people need to live a high-quality life. Insurance companies often cover a large portion of the cost of medical supplies and prescriptions.
Healthcare System Policy-Makers and Regulators
The delivery of health care services is regulated by the federal, state, and local authorities that establish rules to protect the health of the population. The Centers for Medicare and Medicaid Services (CMS) provide government-subsidized medical coverage and set reimbursement standards that regulate the way health care services are organized and delivered in order to ensure the safety, security, and quality of health care services (National Library of Medicine, 2022). The U.S. Department of Health and Human Services (HHS) is the government agency that is responsible for protecting patient privacy, combating fraudulent claims, and ensuring healthcare agencies are compliant with federal laws (DHHS, 2013; Straube, 2013). State medical boards are the agencies that license medical doctors and ensure medical professionals are competent, properly trained, and adhere to the highest standards of excellence (Carlson & Thompson, 2005). Agencies such as the Joint Commission monitor the quality of services by implementing a system that examines healthcare organizations based on compliance and improvement activities (The Joint Commission, 2022; Wadhwa & Huynh, 2021). The Joint Commission grant compliant healthcare organizations with a seal of approval after the organization earns accreditation. These seals are important to healthcare organization because Medicare considers these seals when determining reimbursement (The Joint Commission, 2022; Wadhwa & Huynh, 2021).The government is central to all aspects of healthcare delivery including licensing requirements, standards for participation in government-run programs, security and privacy laws regarding patient health information, and setting standards for patient safety and quality transparency standards of healthcare organizations (Straube, 2013).
Components of the U.S. Healthcare System

|
Knowledge Check Question: Identify and describe the 5 key stakeholders that make up the U.S healthcare system. |
|
Answer: Consumers (patients/recipients of healthcare); insurers and payers (entities responsible for financing healthcare services), Providers (professionals who deliver medical services and care to patients), Suppliers (the companies that supply and distribute medical supplies and medication), Government (the federal, state, and local authorities that establish rules to protect the health of the population). |
|
Factors Impacting Healthcare Delivery and Performance in the U.S.
Although the U.S. has vastly expanded health insurance, barriers to accessibility and affordability remain a challenge plaguing its healthcare system. Nearly 1 in 10 Americans remain without health insurance (Cohen et al., 2022). Individuals without health insurance are more likely to go without needed healthcare services and medications. In fact, nearly 33% of U.S. adults go without recommended healthcare, failed to see a doctor when sick, or did not fill a prescription due to costs. A comparative study, analyzing health policies in 11 developed countries, found that adults in the United States are more likely to go without needed healthcare services due to competing financial demands such as affording basic necessities such as food and housing (Osborn et al., 2016). Unlike the U.S., that utilizes a multi-payer system with competing health insurance companies, most other developed countries operate under a single payer healthcare system where a single public entity finances healthcare for all of its citizens. As a result of the fragmented healthcare system, adults in the U.S. are sicker, experience higher healthcare costs, greater income disparities and are more economically disadvantaged than other high-income nations (Osborn et al., 2016). The U.S. healthcare system is experiencing challenges to its core operations due to increased healthcare spending, shifting patient demands, and varying complex compliance standards.
*The 11 countries: Australia, Canada, France, Germany, the Netherlands, New Zealand, Norway, Sweden, Switzerland, the United Kingdom, and the United States.
Increased Healthcare Spending
The U.S. healthcare system does not have a central agency that plans, directs, and coordinates care leading to a system that is challenged by a duplication of services, waste, inconsistency, and inefficiency due to a lack of systematic planning and cost constraints. Each individual entity comprising the healthcare system seeks to fulfill its own financial agenda. Although the U.S. spends more on healthcare than any other high-income country, this increased spending does not always result in improved healthcare outcomes or a higher functioning health system. The higher spending in the United States is mainly due to higher costs and prices of healthcare, not higher utilization (Tolbert et al., 2020). Despite the heightened spending in the US, still 133 million Americans, nearly half of the U.S. population, suffers from at least one chronic condition and many U.S. adults are not receiving recommended care or necessary preventive and often life-saving screenings for major health conditions (Raghupathi & Raghupathi, 2018; Tolbert et al., 2020). Uninsured individuals, who are unable to pay for routine healthcare services and screenings, often receive care from emergency departments when their conditions have worsened and are the costliest to treat. Increasing access to healthcare will help control the overall cost and burden to the healthcare system.
Further, physician salaries, pharmaceutical prices, and health administrative costs are higher in the U.S. than other developed countries (Papanicolas et al., 2018). For instance, the average salary of generalist physicians in other high-income countries ranges from $86,607 to $157,126, whereas, in the U.S., the average salary is $218,173. Spending per capita on pharmaceuticals was $1,443 in the United States, while the average pharmaceutical costs ranged from $466 to $939 in other countries. Administrative costs, or the costs to plan, direct, and manage healthcare systems accounted for 8% of healthcare spending in the U.S. while the range was 1% to 3% in the other countries (Papanicolas et al., 2018). Overall expenses and uneconomical spending in the U.S. should be controlled through cost control measures and lower administrative costs, as demonstrated by the healthcare systems of other countries.
Shifting Patient Demands
Changing patient demographics contributes to larger gaps in health disparity. As the U.S. population continues to diversify and age, the unique needs and associated conditions (e.g., chronic conditions, literacy barriers, sexual orientation, gender preference) of the population is also changing (Dall et al., 2013). The current population make-up affects healthcare costs, the allocation of necessary resources, and the health and social conditions associated with each subpopulation group (National Association of Health Underwriters, 2015). Consumers of healthcare services have come to expect the same level of automation and convenience in health care as they experience in other segments of the economy. Improved patient experiences and better care coordination will result in improved health outcomes and enhanced satisfaction for care providers as well.
Complex Compliance Regulations
Federal, state, and local governing bodies establish guidelines to protect the health of the population and ensure medical professionals are adhering to the high-quality standards. Healthcare compliance is complex because different bodies govern and set the standards (Field, 2008). Frequent modifications further complicate compliance in healthcare. Healthcare organizations must keep up with changing standards in order to remain compliant. Each change brings new complexities to manage, including shifting expectations and staffing shortages, alongside cost negotiation challenges and coordinating the delivery of quality healthcare services.
|
Knowledge Check Question: Identify and describe the major external forces affecting the delivery of healthcare. |
|
Answer: factors contributing to increased healthcare spending, lack of central agency for planning and coordinating care, shifting patient demands, consequences of uninsured patients reliance on emergency departments, complex compliance regulations |
Historical Overview of the U.S. Healthcare System
The healthcare system in the U.S. has not always been as it is now. In the early years of the U.S. being a formal country, medical care largely lacked a firm foundation in scientific knowledge and principles. Many of the treatments, in fact, caused more harm than benefit to the patients (Rothstein, 1987). For example, physicians frequently used techniques now considered barbaric: bleeding, induced vomiting, and treatment with harmful agents such as mercury (Parascandola, 1976).
Prior to the late 1800s, medical training was much less formal than the large academic institutions of today, with most physicians being trained as apprentices (Rothstein, 1972). Physicians themselves started opening medical schools, in affiliation with nearby universities, increasing the number of formal medical schools from only a small number to more than 40 by the mid-1850s (Rothstein, 1972). Though the number of formal medical schools increased, the quality of education was lacking and many medical schools and insufficient resources for medical education (Starr, 1982).
Hospitals in the early years of the U.S. were also lacking. In fact, what was then called “almshouses,” were simply housing facilities for chronically ill, older adults, those with severe mental illness, individuals with cognitive disabilities, and orphans (Rothstein, 1987). Later, “pest-houses” were created to isolate healthy individuals from those infected with smallpox and other communicable diseases. Caring for the sick was a secondary goal of the pest-houses, the primary goal being isolating health individuals (Rothstein, 1987).
Due to the insufficient care provided by almshouses, physicians started calling for independent hospitals to be established in large cities. This results in Pennsylvania Hospital in Philadelphia, Massachusetts General Hospital in Boston, and New York Hospital in New York City. Unfortunately, though, these first hospitals fell short of their goals and merely supplemented the work of the almshouses rather than replacing it. Long-stays in hospitals were common, with stays of 15 to 40 days not being uncommon (Rothstein, 1987).
The first health insurance plan started in 1929 serving teachers. This model served as the blueprint for the first Blue Cross plans available in the U.S. (Raffel, 1980). However, the concept of insurance coverage began as workers compensation, providing pay to workers who lost work due to job-related injuries or illness. By 1912, many countries in Europe had started national health insurance plans. The U.S., though, resisted this with its entry into World War I as national insurance was thought to be to social insurance, strongly affiliated with German ideals (Starr, 1982).
Aside from the Affordable Care Act, the creation of Medicare and Medicaid is likely the most significant health policy to date. Through Title 18 and Title 19, respectively, of the Social Security Act. Medicare, as you will read more about in later chapters, provides health insurance for older adults while Medicaid provides it for individuals with lower incomes (Starr, 1982).
|
Knowledge Check Question: In your own words, provide a brief summary of the development of the US healthcare system from the early 1800s until present day. In your opinion, what have been the most significant milestones that helped shape the current state of the U.S healthcare system? |
|
Answer: The mid-20th century establishment of employer-sponsored health insurance; Medicare and Medicaid in 1965 expanded healthcare access to the elderly and low-income populations; the Affordable Care Act (ACA) of 2010 aimed to increase access to healthcare through insurance market reforms and Medicaid expansion. The advancements in medical technology have also had a profound impact on shaping the current state of the US healthcare system. The establishment of Medicare and Medicaid, the introduction of the ACA, and advancements in medical technology. |
Conclusion: Bringing Reform to the U.S. Healthcare System
A well-functioning healthcare system should be systematically coordinated, patient-centered, and deliver high quality medical services to all of its consumers. However, in the U.S., healthcare services are rendered to individuals based on ability to pay. Improving the health of the U.S. population will require a more comprehensive and coordinated healthcare delivery system. All individuals should have access to essential and routine medical care services regardless of socioeconomic status, health insurance coverage, geographic location, or race/ethnicity.
Currently, the U.S. medical system focuses on episodic care in the presence of illness or trauma. Value-based care must be a priority in order to lower healthcare costs while providing high quality care. Our healthcare system traditionally rewards doctors for costly treatments and procedures regardless of the value of such treatments. The payment models and structure of the U.S. healthcare system must shift to a valued-based system that incentivizes and encourages disease prevention (Brown & Grossbart, 2019). There are three key ways to shift to a value-based system:
- Best practices, not the costliest. Medical practices, from diagnosis to treatment, should be based on the best available evidence not just the costliest options, without proven heightened positive health outcomes.
- Reduce clinical variation through transparency. Treatment options and costs should be consistent and comparable across healthcare organizations. All healthcare providers and practices should be transparent in their health service costs. Policy changes that would ensure price transparency in healthcare would allow patients to have more control and choice in their health needs and improve competition and lower cost of care.
- Increase patient engagement. Information technology should be implemented to increase clinical collaboration, care coordination, and patient engagement to keep patients aware and involved in their medical care (Brown and Crapo, 2017; Brown & Grossbart, 2019; Miller, 2019). Increasing patient engagement and care coordination will result in improved health outcomes and improved satisfaction for both patients and healthcare providers.
|
Knowledge Check Question: In what ways do patient engagement and the coordination of care contribute to enhancing patient outcomes? |
|
Answer: When patients are actively engaged in their healthcare decisions and treatment plans, they are more likely to understand and adhere to prescribed treatments, medications, and lifestyle changes. By working closely with healthcare providers and care teams, patients can monitor their conditions more effectively, make informed decisions about their care, and prevent complications. Care coordination ensures treatment plans are communicated effectively among healthcare providers, reducing the likelihood of medication errors or conflicting recommendations. Patient engagement initiatives, such as online scheduling and virtual consultations, improve access to healthcare services by reducing wait times and eliminating barriers to care. Coordinated care ensures that patients receive timely and appropriate interventions, reducing the risk of delays in diagnosis or treatment and improving overall health outcomes. |
The performance of a healthcare system are the result of systematic coordination and regulation that increases access while decreasing the cost of medical care. Improving the U.S. healthcare system would result in the narrowing of healthcare gaps for vulnerable groups thereby improving the overall health status of the population.
Case Study Discussion Questions and Answers
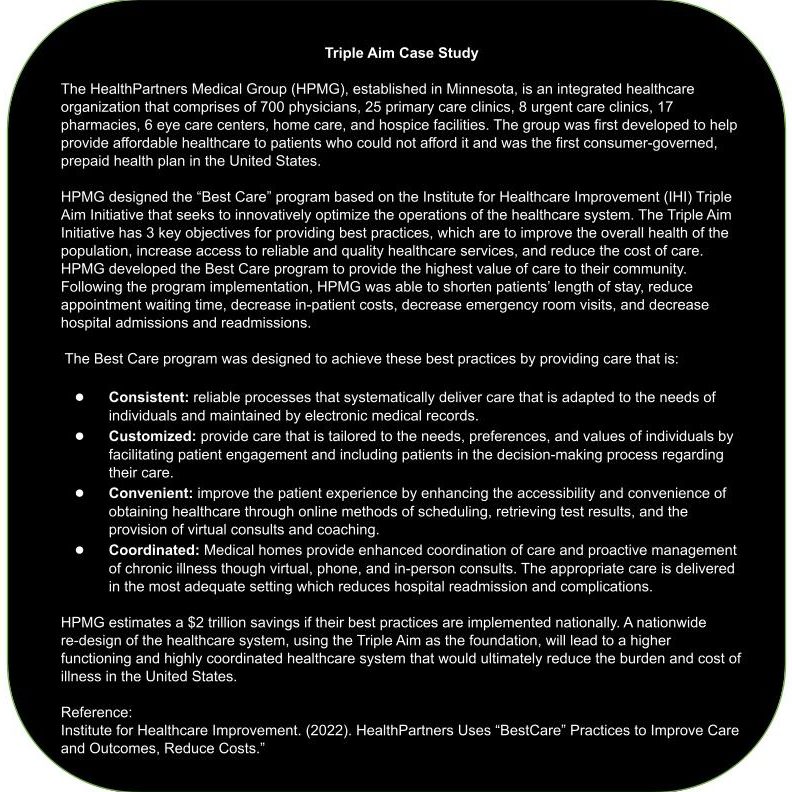
How did HealthPartners Medical Group (HPMG) innovate its operations based on the Institute for Healthcare Improvement’s (IHI) Triple Aim Initiative?
HPMG developed the “Best Care” program to provide the highest value of care to their community, focusing on improving overall population health, increasing access to quality healthcare, and reducing the cost of care. This initiative aimed to optimize healthcare operations by implementing reliable, customized, convenient, and coordinated care practices.
2. What were some of the key objectives of HPMG’s “Best Care” program?
The key objectives of the “Best Care” program included shortening patients’ length of stay, reducing appointment waiting time, decreasing in-patient costs, reducing emergency room visits, and decreasing hospital admissions and re-admissions.
3. How did HPMG achieve the objectives of the “Best Care” program?
HPMG achieved the objectives of the “Best Care” program by implementing consistent, customized, convenient, and coordinated care practices. This involved employing reliable processes, facilitating patient engagement, enhancing accessibility and convenience through online methods, and providing enhanced coordination of care through medical homes.
4. What potential savings did HPMG estimate by implementing their best practices nationally?
HPMG estimated a $2 trillion savings if their best practices were implemented nationally. This suggests that a nationwide re-design of the healthcare system based on the Triple Aim initiative could lead to significant cost reductions and improvements in healthcare outcomes.
5. How might a nationwide re-design of the healthcare system, using the Triple Aim as the foundation, benefit the United States?
A nationwide re-design of the healthcare system based on the Triple Aim initiative could lead to a higher functioning and highly coordinated healthcare system. This could ultimately reduce the burden and cost of illness in the United States while improving overall population health, increasing access to quality healthcare, and reducing healthcare disparities.
Key Terms
Healthcare Consumer: the individuals who are the recipients of healthcare services. They may also be referred to as patients.
In-network provider: a provider who has negotiated rates with the insurance company to provide specific services at a designated rate.
Payers: the private sector, insurance companies; the public sector, government and state agencies; and the consumers, out-of-pocket expenses that share responsibility for healthcare financing.
Third-party payer: any organization that pays or insures health care expenses for the healthcare consumer.
Healthcare Providers: all of the individuals and organizations that provide healthcare services to the consumer.
Healthcare Suppliers: the companies, including the pharmaceutical and medical equipment companies, that supply and distribute medical supplies and medication.
Charge: the designated fee attached to health care services that is set by the provider.
Co-insurance: the designated rate of covered health care services the consumer will pay, set by the third-party payer.
Medicare: a public health insurance provided by the federal government to persons aged 65 and older or individuals under 65 with permanent disabilities
Medicaid: a state-administered health insurance program that provides health care services to low-income families as well as individuals with disabilities.
Children’s Health Insurance Program (CHIP): a state-administered program for low-income children whose families’ earnings disqualify them for Medicaid but still the earnings are inadequate enough to afford private insurance.
TRICARE: a healthcare program for military personnel and their families provided by the Department of Defense
Affordable Care Act (ACA): healthcare reform program that was initiated in 2010 and provided an expansion of health insurance to cover the large number of uninsured individuals in the United States.
Single-payer system: a national health insurance programs run by the government and financed through taxes.
The Centers for Medicare and Medicaid Services (CMS): the federal agency that runs Medicare, Medicaid, and CHIPS programs, providing government-subsidized medical coverage, and sets reimbursement standards that regulate the way health care services are organized and delivered in order to ensure the safety, security, and quality of health care services.
The U.S. Department of Health and Human Services (HHS): is the government agency that is responsible for protecting patient privacy, combating fraudulent claims, and ensuring healthcare agencies are compliant with federal laws.
Joint Commission: is the private agency that monitors the quality of services by implementing a system that examines healthcare organizations based on compliance and improvement activities.
Value-based Care: a system that incentivizes and encourages disease prevention.
References
Berchick, E.R., Hood, E., & Barnett, J.C. (2018). Health Insurance Coverage in the United States: 2017. https://www.census.gov/content/dam/Census/library/publications/2018/demo/p60-264.pdf [PDF – 1.4 MB]
Brown, B., Crapo, J. (2017). The Key to Transitioning from Fee-for-Service to Value-Based Reimbursement. https://www.healthcatalyst.com/wp-content/uploads/2014/08/The-Key-to-Transitioning-from-Fee-for-Service.pdf
Brown, B., & Grossbart, S. (2019). The Top Five 2019 Healthcare Trends. Retrieved March 19, 2020 from https://www.healthcatalyst.com/insights/top-5-2019-healthcare-trends
Carlson, D., Thompson, J.N. (2005). The Role of State Medical Boards. AMA Journal of Ethics, 7(4):311-314. doi: 10.1001/virtualmentor.2005.7.4.pfor1-0504.
Centers for Medicare & Medicaid Services. (2019, November 19). NHE Fact Sheet. Retrieved November 19, 2019, from cms.gov: https://www.cms.gov/research-statistics-data-and-systems/statistics-trends-and-reports/nationalhealthexpenddata/nhe-fact-sheet
Cohen, R.A., Cha, A.E., Terlizzi, E.P., & Martinez, M.E. Health insurance coverage: Early release of estimates from the National Health Interview Survey, 2021. National Center for Health Statistics. May 2022. DOI: https://dx.doi.org/10.15620/cdc:115983.
Dall, T., Gallo, P., Chakrabarti, TW., Semilla a., Storm, M. (2013). “An Aging Population and Growing Disease Burden Will Require A Large and Specialized Health Care Workforce By 2025.” Health Affairs. 32(11): https://doi.org/10.1377/hlthaff.2013.0714
Donnelly, P. D., Erwin, P. C., Fox, D. M., & Grogan, C. (2019). Single-Payer, Multiple-Payer, and State-Based Financing of Health Care: Introduction to the Special Section. American journal of public health, 109(11), 1482–1483. https://doi.org/10.2105/AJPH.2019.305353
Field R. I. (2008). Why is health care regulation so complex?. P & T : a peer-reviewed journal for formulary management, 33(10), 607–608.
Finegold K., Conmy A., Chu R.C., Bosworth A., and Sommers, B.D. Trends in the U.S. Uninsured Population, 2010-2020. (Issue Brief No. HP-2021-02). Washington, DC: Office of the Assistant Secretary for Planning and Evaluation, U.S. Department of Health and Human Services. February 11, 2021.
Health Finance Issues. (2020). National Conference of State Legislators. https://www.ncsl.org/research/health/health-finance-issues.aspx
Institute for Healthcare Improvement. (2022). HealthPartners Uses “BestCare” Practices to Improve Care and Outcomes, Reduce Costs.” http://www.ihi.org/Engage/Initiatives/TripleAim/Documents/IHITripleAimHealthPartnersSummaryofSuccessJul09v2.pdf
Institute of Medicine (US) Roundtable on Evidence-Based Medicine; Yong PL, Saunders RS, Olsen LA, editors. The Healthcare Imperative: Lowering Costs and Improving Outcomes: Workshop Series Summary. Washington (DC): National Academies Press (US); 2010. 20, Consumers-Directed Policies. Available from: https://www.ncbi.nlm.nih.gov/books/NBK53912/
The parts of Medicare (A, B, C, D) (2022). Medicare. https://www.medicareinteractive.org/get-answers/medicare-basics/medicare-coverage-overview/original-medicare
Merriam-Webster. (n.d.). The system. In Merriam-Webster.com dictionary. Retrieved March 21, 2022, from https://www.merriam-webster.com/dictionary/the%20system
Miller, K. (2019). PRACTITIONER APPLICATION Strategies for Delivering Value-Based Care Do Care Management Practices Improve Hospital Performance? Journal of Healthcare Management: November-December 2019 – Volume 64 – Issue 6 – p 445-446
doi: 10.1097/JHM-D-19-00193
National Academy of Engineering (US) and Institute of Medicine (US) Committee on Engineering and the Health Care System; Reid PP, Compton WD, Grossman JH, et al., editors. Building a Better Delivery System: A New Engineering/Health Care Partnership. Washington (DC): National Academies Press (US); 2005. 2, A Framework for a Systems Approach to Health Care Delivery. Available from: https://www.ncbi.nlm.nih.gov/books/NBK22878/
Organization for Economic Co-operation and Development. (2018). Spending on health: latest trends. Accessed at www.oecd.org/health/health-systems/Health-Spending-Latest-Trends-Brief.pdf.
Osborn, R., Squires, D., Doty, MM., Sarnak, DO., Schneider, EC. (2016). 2016 Commonwealth Fund International Health Policy Survey. https://www.commonwealthfund.org/international-health-policy-center/countries/united-states
Papanicolas I, Woskie LR, Jha AK. Health Care Spending in the United States and Other High-Income Countries. JAMA. 2018 Mar 13;319(10):1024-1039. doi: 10.1001/jama.2018.1150. Erratum in: JAMA. 2018 May 1;319(17 ):1824. PMID: 29536101.
PWC Health Research Institute. (2019). Medical cost trend: behind the numbers. Accessed at www.pwc.com/us/en/health-industries/health-research-institute/assets/pdf/hri-behind-the-numbers-2019.pdf
Raghupathi, W., & Raghupathi, V. (2018). An Empirical Study of Chronic Diseases in the United States: A Visual Analytics Approach. International journal of environmental research and public health, 15(3), 431. https://doi.org/10.3390/ijerph15030431
Rosso, RJ. (2021). U.S. Health Care Coverage and Spending. https://sgp.fas.org/crs/misc/IF10830.pdf
Silvers J. B. (2013). The Affordable Care Act: objectives and likely results in an imperfect world. Annals of family medicine, 11(5), 402–405. https://doi.org/10.1370/afm.1567
Slack, WV. Cybermedicine: How Computing Empowers Doctors and Patients for better Health Care. Jossey-Bass 2001.
Straube, BM. (2013). A Role for Government: An Observation on Federal Healthcare Efforts in Prevention. American Journal of Preventive Medicine. DOI:https://doi.org/10.1016/j.amepre.2012.09.009
The Affordable Care Act: A Brief Summary. (2011). National Conference of State Legislators. https://www.ncsl.org/research/health/the-affordable-care-act-brief-summary.aspx
The Joint Commission. (2022). The Gold Seal of Approval and Guidelines for Use. https://www.jointcommission.org/accreditation-and-certification/accredited/publicity-kit/the-gold-seal-of-approval-and-guidelines-for-use/
Tikkanen, R., Osborn, R., Mossialos, E., Djordjevic, A., & Wharton, G. (2022). International Health Care System Profiles, United States. The Commonwealth Fund. https://www.commonwealthfund.org/international-health-policy-center/countries/united-states
Tolbert, J., Orgera, K., Damico, A. 2020. Key Facts about the Uninsured Population.
https://www.kff.org/uninsured/issue-brief/key-facts-about-the-uninsured-population/
US Department of Health and Human Services. (2013). About the Law. http://www.hhs.gov/healthcare/rights/index.html.
Wadhwa R, Huynh AP. The Joint Commission. [Updated 2021 Mar 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557846/
Wager, E., Ortaliza, J., Cox, C. (2022). How does health spending in the U.S. compare to other countries? Peterson-KFF Health system. https://www.healthsystemtracker.org/chart-collection/health-spending-u-s-compare-countries-2/
World Health Organization. (2010). Key components of a well-functioning health system. https://www.who.int/healthsystems/EN_HSSkeycomponents.pdf