12
Historic and Future Perspectives in Healthcare Information Technology
Mary A. Moore, PhD
Colorado State University Global
“The best way to predict the future is to create it” – Alan Kay
Learning Objectives
- Understand the history of medical records and technology use in healthcare.
- Understand the factors that have influenced healthcare reform.
- Explain the importance of patient engagement to patient outcomes.
- Describe the innovative technologies and standards that support safe and effective patient care.
- Discuss the system acquisition process from a project management perspective.
Introduction
Medical records have been kept since ancient times as archaeologists have found clay tablets and other writing media in Mesopotamia in the Middle East, Egypt, Greece, and Rome (Bjelica, 2017). Today the medical environment is supported by digital technologies that allow us to create and maintain an electronic health record that records patient illness, treatments, and treatment outcomes. With the emergence of minicomputers in the late 1970s, the use of computers supported the automation of many administrative processes and functions of clinical applications for billing, laboratory, pharmacy, and radiology (Thede & Sewell, 2012). The adoption of the computerized electronic health record provides the opportunity to streamline processes and create greater efficiency, however, there continues to be challenges of inadequate user interfaces and the computer.
The Institute of Medicine (IOM) created a report “To Err Is Human: Building a Safer Health System” (1999) that identified preventable medical errors (in 2015 the name changed from Institute of Medicine to the National Academy of Medicine). In 2001 the Institute of Medicine released another study “Crossing the Quality Chasm: A New Health System for the 21st Century” that identified six aims for the improvement of patient care. These two studies became the foundation of healthcare reform in the United States. The need for healthcare reform was one of the many reasons that the American Recovery and Reinvestment Act (ARRA) was signed into law in 2009 by President Obama to modernize the nation’s infrastructure, the energy sector, expanded educational opportunities, and improvements in affordable healthcare. The Health Information and Technology for Economic and Clinical Health (HITECH) Act was a part of ARRA and was designed to expand the adoption of health information technology such as the use of electronic health records by providing funding through incentive payments authorized by Medicare and Medicaid to be paid to hospitals and clinicians who could demonstrate the meaningful use of EHRs (Excite Health Partners, 2012). The EHR incentives were available to eligible care providers who met the criteria defined by Medicare and Medicaid and ended in 2016. Medicare incentives were available to hospitals that received payments under the Inpatient Prospective Payment System (IPPS), critical access hospitals, and Medicare advantage. The eligible professionals were medical or osteopathy doctors, dental surgeons, podiatrists, doctors of optometry, and chiropractors. Medicaid incentives were available to acute care, critical access, children, and cancer hospitals that served at least 10% of their patient volume made up of Medicaid patients. Eligible professionals are physicians, nurse practitioners, certified nurse-midwives, dentists, and physician assistants working in a federally qualified health center or rural health clinic (CMS, 2010). To be eligible for the incentive payments the participants must demonstrate the meaningful use of the certified EHR to improve the quality of healthcare by achieving clinical quality measures.
We have many technologies that have been developed such as electronic health records that provide patient portals for better communication between patients and their primary care providers. COVID-19 disrupted many aspects of patient access to care and fortunately, telehealth services and remote monitoring allowed patients to receive care while reducing their risk of exposure to the disease (Brotman & Kotloff, 2021). The Office of the National Coordinator (ONC) for Health Information Technology (HIT) provides guidance according to a set of standards that let healthcare organizations connect their systems so that patient data can be shared securely in a variety of health information exchange scenarios. The ONC helps overcome HIT challenges by developing standards and implementation guidance for interoperability between information systems (HealthIT, 2019). In this chapter, we will explore these topics in much greater depth.
Questions:
What were the two IOM reports? Answer: To Err Is Human: Building a Safer Health System and Crossing the Quality Chasm: A New Health System for the 21st Century.
What healthcare reform legislation led to improvements in affordable healthcare? Answer: The American Recovery and Reinvestment Act (ARRA).
What healthcare legislation was designed to expand the adoption of health information technologies such as the electronic health record? Answer: The Health Information and Technology for Economic and Clinical Health (HITECH) Act.
What did eligible professionals do to receive EHR incentive money? Answer: They demonstrated the meaningful use of a certified EHR to improve the quality of healthcare using clinical quality measures.
What feature in an EHR provides better communication between patients and their primary care providers? Answer: The patient portal.
History of Technology in the Healthcare Setting
For many centuries, observations have been made by individuals like Hippocrates who lived 460-370 BCE where he emphasized observation and the importance of nutrition in the health of an individual (Jones, 1868). Throughout history, the observations of healers were recorded along with any treatments they provided. This effort to document successful treatments helped improve the selection of effective treatments that would improve the health of those being treated by sharing this knowledge with other healers.
Fast forward to the 20th century, the American College of Surgeons (ACS) created the Association of Record Librarians of North America in 1928 to standardize paper medical record documentation. The ACS began creating rigorous standards for clinical records used in medical institutions. The purpose was to ensure the accurate capture of clinical data in settings ranging from the physician office to the hospital. The availability of health information provides the continuity of care needed for the patient (AHIMA, 2021).
The need to collect accurate medical records was supported by new technologies such as computers. In the late 1950s through the mid-1960s second generation computers were based on transistors, and became smaller and faster than the earlier first-generation computers that used vacuum tube and took up large areas within a building. Third generation computers used the integrated circuit and were followed by fourth generation computers using microprocessor chips developed by Intel in the 1970s. As the demands for computing power and speed increased to handle large amounts of data, computers became smaller and faster to accommodate these needs (Thede & Sewell, 2012).
The Mayo Clinic in Rochester, Minnesota was one of the first healthcare organizations to adopt electronic medical records according to the National Institutes of Health. The Department of Defense implemented a hospital computer program in the 1970s that would become the VistA (Veterans Health Information Systems and Technology Architecture) electronic health record (WorldVistA, 2004). The primary barriers to the adoption of electronic medical records were the cost of those systems and the lack of robust data standards.
1990s
In the early 1990s, less than 20 percent of physician practices were using a computer-based medical record. In 1991, the Institute of Medicine (IOM) presented a goal published in The National Academies Press (NAP), with the recommendation that all physicians should be using computer-based patient records in their practices (IOM, 1999; IOM, 2001). The goal of the electronic health record was to improve the quality and safety of patient care.
One important consideration is that the terms electronic medical record and electronic health record are not interchangeable. There is an important difference between the electronic medical record (EMR) and the electronic health record (EHR). The EMR, based on the paper chart, includes the history and physical (H&P), diagnoses, medications, immunizations, and allergies of each patient in an electronic format. The problem with this format is that the information contained in the EMR is not structured data available in a searchable database since some of the information could include optically scanned paper charts. The EHR gathers discrete and structured data that is searchable in a database. The EMR is a digital form of a paper chart and contains the same medical information about a patient’s medical and treatment history for that physician’s practice. Like paper, they track patient data such as illnesses, blood pressure readings, and vaccinations (Garrett & Seidman, 2011). The EHR allows healthcare providers to use linked clinical decision support tools including health information collected outside the single practice setting. This ability to share patient information using an EHR provides a continuity of care for the patient and improved clinical decision-making for authorized clinicians in multiple healthcare organizations.
At the end of the 1990s and early 2000s two ground breaking studies were released by the IOM that reported on medical errors and the harm that patients suffered as a result of seeking medical treatment. The IOM studies were the catalyst for our current focus on patient safety and improvements in the quality of care. The first report “To Err Is Human: Building a Safer Health System” (1999) found that 44,000 to as many as 98,000 patients die each year from preventable medical errors. The types of errors identified in the IOM report include diagnostic, treatment, and prevention. Diagnostic errors result from the delay of diagnosis, incorrect testing, or not using evidence-based therapies. The failure to act on the data provided by patient monitoring or testing is an error. Treatment errors include the incorrect performance of a test, procedure, operation, or the delay in responding to an abnormal test result by administering appropriate treatment or treatments not indicated for the patient’s condition. Prophylactic treatments are provided for the benefit of the patient based on the clinical evidence available. Preventive measures include adequate monitoring or follow-up treatments and communication. Additional errors can be the result of equipment or system failures. The majority of medical errors are not due to recklessness, but are caused by inadequate “systems, processes, and conditions that lead people to make mistakes or fail to prevent them” (IOM, 1999, p.2). The IOM identified eight EHR capabilities to overcome the inadequacies of these systems and processes.
Eight critical core EHR capabilities identified by the Institute of Medicine:
Health information and data – Current patient information available at the point of care pulls all related medical and diagnostic information from integrated clinical decision-support systems includes diagnosis, lab results, and current medications.
Result management – The capability of electronic reporting of all medical and diagnostic information currently available on the patient including historical data.
Order management – Electronic order entry into a database that is capable of storing orders for services, tests, or prescriptions in a computer-based system that increases legibility, checks for order duplication, and improves the speed that the orders are processed.
Decision support – Clinical-decision support systems provide reminders, evidence-based best practice information, prompts, and alerts such as medication interactions that help avoid adverse medication events. Information from clinical-decision support systems include all aspects of disease management such as disease outbreaks in geographic locations.
Electronic communication and connectivity – The ability to communicate electronically between healthcare providers and patients securely and efficiently supports better care and allows the exchange of healthcare data between providers that supports the continuity of care. We have seen a rise in the use of telemedicine and remote monitoring capabilities that improve access to care.
Patient support – Patient portals provide the ability to provide patient education, allow access to patient records, and test results. Remote monitoring is a powerful tool to let the patient report blood pressure, fasting blood sugars, or other readings the care provider needs in order to manage their chronic conditions.
Administrative processes – The electronic tools available in these systems support administrative processes that include scheduling and billing. These systems also help to improve the efficient and timely provision of services to patients.
Reporting – Since patient data is stored electronically, the systems must conform to uniform data standards and help health care organizations support patient safety and perform disease surveillance (Digital Health, 2021).
Also in the 1990s, we saw the development and implementation of healthcare policies and information standards that helped healthcare organizations to develop a patient safety culture based on the clinical evidence. System design helps to improve processes for safe working conditions through a workflow analysis (IOM, 1999). Improving medication safety includes changes in the medication administration process by incorporating medication dispensing cabinets, barcode medication administration, and smart pumps. According to Tompkins McMahon (2017), work interruptions present a danger during medication administration. This understanding helps organizations prioritize the reduction of interruptions and distractions in order to limit the risk of medication administration errors. Professional nursing and medical societies develop standards for their members to improve their approach to patient safety and performance in their clinical practice.
2000-2010
In 2001, the Institute of Medicine released another study “Crossing the Quality Chasm: A New Health System for the 21st Century” which identified six aims to improve healthcare: safe, effective, patient-centered, timely, efficient, and equitable care. The Institute for Healthcare Improvement (IHI) also provided 10 rules for the redesign of healthcare delivery systems: 1) “Change the balance of power by creating a partnership with patients, families, and communities; 2) Standardize what is possible to reduce unnecessary variation and increase the time available for individualized care; 3) Customize care to the individual’s needs, values, and preferences, guided by and understanding of what matters to the person in addition to “What’s the matter?”; 4) Promote well-being by focusing on outcomes that matter the most to people appreciating that their health and happiness may not require healthcare; 5) Create joy in work by cultivating and mobilizing the pride and joy of the healthcare workforce; 6) Make it easy, continually reduce waste and all nonvalue-added requirements and activities for patients, families, and clinicians; 7) Move knowledge, not people by exploiting all helpful capacities of modern digital care and continually substitute better alternatives for visits and institutional stays- meet people where they are; 8) Collaborate and cooperate by recognizing that the healthcare system is embedded in a network that extends beyond traditional walls by eliminating knowledge/information silos, institutional or professional boundaries that impeded flow and responsiveness; 9) Assume abundance by using all the assets that can help to optimize the social, economic, and physical environment, especially those brought by patients, families, and communities; and 10) Return the money by giving the money from healthcare savings to other public and private purposes (IHI, 2015). Customized healthcare that meets the patient needs considers their values by responding to their choices or preferences. Patients must have the necessary information regarding their condition and treatment options to control their healthcare decisions and participate in collaborative decision-making with their care providers. Patients must have access to their medical information and the ability to communicate with their primary care providers if they have questions.
Healthcare decision-making is based on the current scientific knowledge available to provide evidence-based decision-making and is important in improving the quality and safety of patient care as discussed in the IOM reports. The healthcare system must be designed to reduce the risk of injury by preventing and mitigating potential process errors and engaging the patient as part of the care team that coordinates care and shares needed patient information that supports collaboration between all healthcare providers so that better patient outcomes are achieved.
Six Domains (Aims) of Healthcare Quality
- Safe: avoiding injuries to patients from the care that is intended to help them.
- Effective: providing services based on scientific knowledge to all who could benefit, and refraining from providing services to those not likely to benefit.
- Patient-centered: providing care that is respectful of and responsive to individual patient preferences, needs, and values, and ensuring that patient values guide all clinical decisions.
- Timely: reducing waits and sometimes harmful delays for both those who receive and those who give care.
- Efficient: avoiding waste, including waste of equipment, supplies, ideas, and energy.
- Equitable: providing care that does not vary in quality because of personal characteristics such as gender, ethnicity, geographic location, and socioeconomic status” (IOM, 2001, p.3).
These quality domains are important quality measures that organizations can apply and can be summarized by measuring safe, effective, patient-centered care that are an understandable grouping of the six aims.
2010 to the present
After the passage of the American Recovery and Reinvestment Act in 2009 healthcare providers were required to adopt EHRs (Denis et al., 2012). The Health Information Technology for Economic and Clinical Health (HITECH) Act was an important part of the American Recovery and Reinvestment Act of 2009 (HHS, 2017). HITECH strengthened privacy and security by providing civil and criminal penalties for HIPAA (Health Insurance Portability and Accountability Act) (CDC, 2018) violations. The challenges with EHR adoption continue to be the integration of legacy systems with new EHR and clinical decision support technologies.
The challenges healthcare organizations face once an EHR is adopted is the use and sharing of patient information in a meaningful way to improve patient care and reduce the costs of that care. Healthcare providers who want to participate in a health information exchange (HIE) must be using a certified EHR. Current research indicates that the participation in a HIE improves the organization’s performance regarding readmissions, a reduction in the cost of lab test, diagnostic imaging, and other costs of care resulting in a return on investment (Menachemi, et al. 2018). The goal of a nation-wide HIE has several barriers: information technology infrastructure such as fiber internet is not robust or widespread enough to support this goal, especially in rural areas, all healthcare providers must adopt the EHR, and the challenges of legacy systems and interoperability must be overcome.
Healthcare Information Systems Interoperability
HIMSS (Health Information Management Systems Society) describes four levels of interoperability:
- Foundational (Level 1): Establishes the inter-connectivity requirements needed for one system or application to securely communicate data to and receive data from another.
- Structural (Level 2): Defines the format, syntax and organization of data exchange including at the data field level for interpretation.
- Semantic (Level 3): Provides for common underlying models and codification of the data including the use of data elements with standardized definitions from publicly available value sets and coding vocabularies, providing shared understanding and meaning to the user.
- Organizational (Level 4): Includes governance, policy, social, legal and organizational considerations to facilitate the secure, seamless and timely communication and use of data both within and between organizations, entities and individuals. These components enable shared consent, trust and integrated end-user processes and workflows” (HIMSS, 2021, para. 2).
Questions:
When were paper medical records standardized? Answer: 1928 when the American College of Surgeons created the Association of Record Librarians of North America.
Who was the first healthcare organization to adopt medical records? Answer: Mayo Clinic in Rochester, Minnesota.
What was the catalyst for patient safety and improvements in the quality of care? Answer: The Institute of Medicine studies.
What are the six aims of healthcare quality? Answer: Safe, effective, patient-centered, timely, efficient, and equitable care.
What barriers prevent the achievement of a nation-wide HIE? Answer: Information technology infrastructure, EHR adoption, and interoperability between legacy information systems.
Now that we have reviewed the issues of interoperability, we need to look at information system standards.
Information System Standards
The electronic health record must be able to efficiently capture patient data and share it with other health care providers. This capability depends on structured data that allows the retrieval of that data as needed for patient care. The Centers for Medicare and Medicaid Services (CMS) and the Office of the National Coordinator for Health Information Technology (ONC) worked together to establish the structured data standards. The new updates to the Certified Electronic Health Record Technology (CEHRT) requirements include promoting interoperability, quality payment, and hospital inpatient quality reporting identified in the 21st Century Cures Act (section III.M.). The vision of the ONC is to make it easier for patients to view their health records on smartphones as well as enhancing privacy and security requirements to protect their health information (CMS, 2021b).
Health Level Seven (HL7) founded in 1987, provides the standards needed to integrate, share, exchange, and retrieve electronic health information. HL7 standards address language, data structure, and types so information systems can integrate and support health care organizations and providers in the delivery of health services.
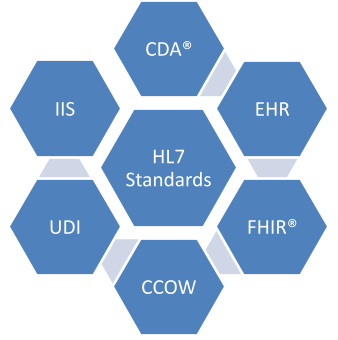
There are several groups of standards: 1) Clinical Document Architecture/ Clinical and Administrative Domains (CDA®), 2) Electronic Health Records (EHR), 3) Fast Healthcare Interoperability Resources (FHIR®), 4) Clinical Context Management Specification (CCOW), 5) Cross-paradigm/Domain Analysis Models (UDI), 6) Implementation Guides (IIS), and 7) Rules and References. The standards for system integration, technical, programming, and guidelines for software and standards development are needed to improve the integration and implementation of health information systems (HL7, 2021).
The importance of standardization is highly related to data quality and we must consider that these standards help us to secure our internal networks and make it possible to communicate over the Internet. Beginning with the Internet standards, they are based on many different standards that help us share information. The Transfer Control Protocol/Internet Protocol (TCP/IP) is used to communicate on a private computer network called an intranet. TCP/IP is made up of two protocols where TCP defines how applications can communicate on the network by managing discrete data packets for transmission and then reassembles them in the right order when they reach their intended destination. IP defines how to address and route each of the packets by providing an IP address so it arrives at the correct destination. Simple Mail Transfer Protocol (SMTP) is an application layer protocol that uses TCP to open a connection to the SMTP server and then can send an email across that connection. Hyper Text Markup Language (HTML) is the language that helps you write webpages and websites and controls color, font, pictures, and everything else we see online.
The process of standardization provides a framework for semantic interoperability since there must be messaging standards such as Health Level Seven (HL7) that is a set of clinical standards and messaging formats that helps integrate, exchange, and retrieve electronic information across different healthcare information systems, especially legacy information systems that need to be connected to a new EHR. Digital Imaging and Communications in Medicine (DICOM) is a standard for handling, storing, printing, and transmitting the information contained in medical imaging (Sachdeva et al., 2012). The Web Ontology Language is based on Description Logistics and are Semantic Web technologies that support machine to machine communication so that data can be shared (Legaz-García et al., 2016). The Systemized Nomenclature of Medicine-Clinical Terms (SNOMED CT®) is a standardized clinical terminology that was developed by the College of American Pathologists. SNOMED CT® was approved in 2003 by the Department of Health and Human Services (IOM, 2005; Truran et al., 2010; Willett et al., 2018). SNOMED CT® defines diseases, procedures, and organisms, however, computers and EHRs only understand structured data, so abbreviations that a human could interpret cannot be used since abbreviations are not structured. As we share more health information between healthcare professionals, the importance of semantic interoperability becomes clear (Choi et al. 2005; Goodenough, 2009; Ullah et al, 2017). With this in mind, it is important we understand the purpose of the standard setting organizations involved in the exchange of health information.
Standard Setting Organizations
- AHRQ – Agency for Healthcare Research and Quality (www.ahrq.gov) The AHRQ’s mission is to improve the quality, safety, efficiency, and effectiveness of health care for all Americans.
- AHIMA – American Health Information Management Association (www.ahima.org) AHIMA was founded in 1928 to improve the quality of medical records.
- AMIA – American Medical Informatics Association (www.amia.org) AMIA helps advance the use of health information and communications technology (HICT) in clinical care and research, public and population health.
- ANIA – American Nursing Informatics Association (www.ania.org) The ANIA provides networking, education and information resources that enrich and strengthen the roles of nurses in the field of informatics that includes the domains of clinical information, education, and administration decision support.
- ANSI – American National Standards Institute (www.ansi.org) ANSI enhances both the global competitiveness of U.S. business and the U.S. quality of life by promoting and facilitating voluntary consensus standards and conformity assessment systems, and safeguarding their integrity.
- ASC X12 – The Accredited Standards Committee X12 (www.x12.org) ASC X12 is an innovative leader in the development of cross industry e-commerce standards that improve global business process interoperability and facilitate business information exchange.
- ASTM – American Standards Testing and Materials (www.astm.org) ASTM International, originally known as the American Society for Testing and Materials (ASTM), is one of the largest voluntary standards development organizations in the world. ASTM is a trusted source for technical standards for materials, products, systems, and services. Known for their high technical quality and market relevancy, ASTM International standards have an important role in the information infrastructure that guides design, manufacturing, and trade in the global economy.
- ATA – American Telemedicine Association (www.atmeda.org) The American Telemedicine Association is the leading resource and advocate promoting access to medical care for consumers and health professionals via telecommunications technology. ATA seeks to bring together diverse groups from traditional medicine, academic medical centers, technology and telecommunications companies, e-health, medical societies, government, and others to overcome barriers to the advancement of telemedicine through the professional, ethical, and equitable improvement in health care delivery.
- CAQH – Council for Affordable Quality Healthcare (www.caqh.org) An unprecedented nonprofit alliance of health plans and trade associations, is a catalyst for industry collaboration on initiatives that simplify healthcare administration. CAQH solutions promote quality interactions between plans, providers, and other stakeholders; reduce costs and frustrations associated with healthcare administration; facilitate administrative healthcare information exchange and encourage administrative and clinical data integration.
- CCHIT – Certification Commission for Health Information Technology (www.cchit.org) The Certification Commission for Healthcare Information Technology or CCHIT is a recognized certification body (RCB) for electronic health records and their networks, and an independent, voluntary, private-sector initiative. Its mission is to accelerate the adoption of health information technology by creating an efficient, credible, and sustainable certification program.
- eHI – eHealth Initiative (www.ehealthinitiative.org) The eHealth Initiative and the Foundation for eHealth Initiative are independent, non-profit affiliated organizations whose missions are the same: to drive improvement in the quality, safety, and efficiency of healthcare through information and information technology. Both organizations are focused on engaging multiple and diverse stakeholders to define and implement actions to address quality, safety and efficiency challenges of our healthcare system through the use of interoperable information technology.
- GS1 US – (www.gs1us.org) GS1 is a fully integrated global standards organization with 108 member organizations representing 150 countries worldwide. GS1 US leads its North American membership with true global representation in the GS1 System.
- HIMSS – Healthcare Information and Management Systems Society (www.himss.org) HIMSS is the healthcare industry’s membership organization exclusively focused on providing leadership for the optimal use of healthcare information technology (IT) and management systems for the betterment of healthcare.
- HITSP – The Healthcare Information Technology Standards Panel (www.hitsp.org) HITSP is a cooperative partnership between the public and private sectors. The Panel was formed for the purpose of harmonizing and integrating standards that will meet clinical and business needs for sharing information among organizations and systems.
- HL7 – Health Level Seven (www.hl7.org) HL7 is one of several American National Standards Institute (ANSI) -accredited Standards Developing Organizations (SDOs) operating in the healthcare arena. Health Level Seven is a not-for-profit volunteer organization. Its members– providers, vendors, payers, consultants, government groups and others who have an interest in the development and advancement of clinical and administrative standards for healthcare—develop the standards. Health Level Seven adheres to a strict and well-defined set of operating procedures that ensures consensus, openness and balance of interest. Health Level Seven develops specifications, the most widely used being a messaging standard that enables disparate healthcare applications to exchange key sets of clinical and administrative data.
- NCPDP – National Council for Prescription Drug Programs (www.ncpdp.org) NCPDP creates and promotes standards for the transfer of data to and from the pharmacy services sector of the healthcare industry. The organization provides a forum and support wherein our diverse membership can efficiently and effectively develop and maintain these standards through a consensus building process. NCPDP also offers its members resources, including educational opportunities and database services, to better manage their businesses.
- NCVHS – National Committee for Vital and Health Statistics (www.ncvhs.hhs.gov) The National Committee on Vital and Health Statistics was established by Congress to serve as an advisory body to the Department of Health and Human Services on health data, statistics and national health information policy. It fulfills important review and advisory functions relative to health data and statistical problems of national and international interest, stimulates or conducts studies of such problems and makes proposals for improvement of the Nation’s health statistics and information systems. In 1996, the Committee was restructured to meet expanded responsibilities under the Health Insurance Portability and Accountability Act of 1996 (HIPAA).
- NIST – National Institute of Standards and Technology (www.nist.gov) Founded in 1901, NIST is a non-regulatory federal agency within the U.S. Department of Commerce. NIST’s mission is to promote U.S. innovation and industrial competitiveness by advancing measurement science, standards, and technology in ways that enhance economic security and improve our quality of life.
- NLM – National Library of Medicine (www.nlm.nih.gov) The National Library of Medicine (NLM), on the campus of the National Institutes of Health in Bethesda, Maryland, is the world’s largest medical library. The Library collects materials and provides information and research services in all areas of biomedicine and health care.
- ONC – Office of the National Coordinator for Health Information Technology (www.healthit.gov) The National Coordinator for Health Information Technology serves as the Secretary’s principal advisor on the development, application, and use of health information technology; coordinates the Department of Health and Human Services’ (HHS) health information technology programs; ensures that HHS health information technology policy and programs are coordinated with those of other relevant executive branch agencies; and to the extent permitted by law, develops, maintains, and directs the implementation of a strategic plan to guide the nationwide implementation of interoperable health information technology in both the public and private health care sectors that will reduce medical errors, improve quality, and produce greater value for health care expenditures, and coordinates outreach and consultation by the relevant executive branch agencies with the public and private sectors.
- WEDI – Workgroup for Electronic Data Interchange (www.wedi.org) The WEDI provides leadership and guidance to the healthcare industry on how to use and leverage the industry’s collective knowledge, expertise and information resources to improve the quality, affordability and availability of healthcare” (AMCP, 2021, p. 1).
Questions:
What standards address integration and exchange of electronic health information? Answer: Health Level Seven (HL7).
What is the importance of data standards? Answer: Standards help to secure an organization’s internal network and communication of high-quality data over the Internet.
What protocol defines how applications communicate on a network? Answer: The Transfer Control Protocol (TCP).
What protocol defines how to address and route each of the data packets by providing an address so it arrives at the correct destination? Answer: Internet Protocol (IP).
What are DICOM and SNOWMED CT examples of? Answer: Clinical standards and messaging formats for the exchange of electronic clinical information.
Healthcare Legislation
Healthcare legislation is created to improve access to care and our modern delivery of that care depends on the use of the information technologies that we have available at the point of care. Our EHRs are connected to the Internet, and from that perspective we must be concerned with protected health information (PHI) so that it is secure when used or shared with other healthcare providers. When we consider the ARRA legislation in 2009 that included HITECH (Health Information Technology for Economic and Clinical Health) Act, we were able to strengthen HIPAA security through the fines and penalties that HITECH introduced to manage data breaches.
The HITECH Act of 2009 that was part of ARRA 2009 that provided Health and Human Services authority to create programs that would improve healthcare quality, safety, and efficiency in the exchange of health information. The barriers identified by the HITECH Act were commercial, economic, and technical barriers (HealthIT, 2013). HITECH expanded the adoption of health information technology such as EHRs by providing funding through incentive payments authorized by Medicare and Medicaid to hospitals and clinicians who could demonstrate the meaningful use of EHRs by integrating clinical quality measures in patient care (Excite Health Partners, 2012; HealthIT, 2015). According to the HIPAA Journal (2022) HITECH not only encouraged the adoption of Certified EHRs (HealthIT, 2015) but also removed loopholes in HIPAA by making the language describing HIPAA Rules more robust. HITECH applied the HIPAA Security and Privacy Rules to business associates so that they were legally responsible for HIPAA compliance just as the covered entities are, we will be discussing covered entities in the next section. With the increased adoption of EHRs to gather patient health information, there is an increased vulnerability of data breaches. HIPAA administrative, technical, and physical safeguards must be implemented so that the protected health information (PHI) is kept confidential, private, and secure (HealthIT, 2017).
The EHR incentives were available to eligible care providers who met the criteria defined by Medicare and Medicaid and began in 2011 and continued through 2016 (Burke, 2010). The Medicare incentives were available to hospitals that received payments under the Inpatient Prospective Payment System (IPPS), critical access hospitals, and Medicare advantage. The eligible professionals were medical or osteopathy doctors, dental surgeons, podiatrists, doctors of optometry, and chiropractors. Medicaid incentives were available to acute care, critical access, children’s hospitals and cancer hospitals that served at least 10% of their patient volume made up of Medicaid patients. Eligible professionals are physicians, nurse practitioners, certified nurse-midwives, dentists, and physician assistants working in a federally qualified health center or rural health clinic (CMS, 2010). To be eligible for the incentive payments the participants must demonstrate the meaningful use of the certified EHR to improve the quality of healthcare by achieving clinical quality measures to meet meaningful use objectives. Meaningful use included privacy and security requirements that PHI would be protected from unauthorized access and that the patients would have access to their medical information (HealthIT, 2015).
HIPAA Background
The Health Insurance Portability and Accountability Act (HIPAA) privacy and security rules grew out of two statutes in the 1970’s that addressed the concerns for confidential patient information. First the Comprehensive Alcohol Abuse and Alcoholism Prevention, Treatment, and Rehabilitation Act of 1970 and the Drug Abuse Prevention, Treatment, and Rehabilitation Act of 1972 (HHS, 1994). Protecting the identities of people seeking treatment for addiction was a catalyst for our “current need to know” policies that define many of our information security strategies. The Health Insurance Portability and Accountability Act (HIPAA) signed into law in 1996 by President Bill Clinton. This act protects the health insurance coverage of people when they change or lose their employment. HIPAA created standards for electronic healthcare transaction along with national identifiers for healthcare providers, insurers, and employers (HealthIT, 2021a). At this point, it is important to review the privacy and security standards identified with HIPAA:
HIPAA Privacy and Security Standards
“HIPAA Privacy Rule: Establishes national standards to protect individuals’ medical records and other personal health information. It applies to health plans, healthcare clearinghouses, and healthcare providers that conduct certain healthcare transactions electrically. The rule applies safeguards to protect the privacy of personal health information, and sets limits and conditions on the uses and disclosures of such information without patient authorization. The rule also gives patient’s rights over their own health information, including the right to examine and obtain a copy of their records, and to request corrections.
HIPAA Security Rule: Sets national standards for protecting the confidentiality, integrity, and availability of electronically protected health information. Compliance with the Security Rule was required as of April 20, 2005 (April 20, 2006 for small health plans). The rule addresses the technical and non-technical safeguards that “covered entities” must have in place to secure an individual’s electronic protected health information. Prior to HIPAA, there were no generally accepted requirements or security standards for protecting health information” (HIMSS, 2021, para. 9).
Covered Entities
The protection of electronic patient information requires a definition of who is required to follow HIPAA privacy and security requirements. This is important since only a covered entity is required to be HIPAA compliant and responsible for data breaches. CMS defines a covered entity as any entity that provides, bills, or receives payments for healthcare services as part of their normal business activities. If a clearinghouse processes or facilitates the processing of health information from nonstandard or standard formats into standard or nonstandard formats, this qualifies them as a covered entity. Private group healthcare benefit plans and insurers that provide or pay for the cost of medical care qualify these groups as a covered entity. An exception is if the benefit plan has less than 50 participants and is self-administered, then it is not a covered entity. Supplemental Medicare policies and health maintenance organizations (HMOs) are covered entities. Considering these definitions, health insurance companies, HMOs, employer-sponsored health plans, Medicare, Medicaid, military, and veteran’s health programs are covered entities. Health Data Clearinghouses, doctors, clinics, psychologists, dentists, chiropractors, nursing homes, and pharmacies are all covered entities. This brings up the consideration that if a covered entity uses the services of a third party such as a Cloud Service Provider, they must have a written business associate’s agreement (BAA) contract that establishes what this third party has been engaged to do and the BAA states that they must comply with HIPAA regulations. Some other examples are a third-party that helps with health plan claims processing, utilization review consultants, and independent medical transcriptionist services for physicians (CMS, 2021a).
CMS HIPAA Safeguards
Before HIPAA became law in 1996, there was no accepted standard for protecting health information. CMS outlined the policies and procedures needed to protect patient information set out here. Security is certainly one of the primary concerns organizations have in protecting patient health information (PHI) as well as sharing it with other organizations in heath information exchanges for example. There are three security safeguards used to secure an organization’s protected health data: administrative, physical, and technical. Administrative safeguards demonstrate appropriate written policies, procedures, and job descriptions are in place including sanctions for violations so staff are aware of their HIPAA responsibilities and can be properly trained. Physical safeguards define user access, training, disaster planning, backup, facility inventory, safeguards for unauthorized physical access or tampering, and contingency plans. Technical controls include unique user identification, password policies, user access allowed, automatic log off, email policies, encryption, and data transmission protocols. Considering organizational requirements, they must include the use of Business Associates Agreements (BAAs) that identify and control the amount of access that a vendor could have to protected health information (CMS, 2016).
Threats to Protected Healthcare Information
Inside the healthcare organization, the need for security training for all staff accessing the information system is critical to protecting health information. The threats to information security can be intentional or unintentional. The threat source is either internal to the organization or external to the organization. An intentional exposure of patient information without authorization can be the result of a hacker or a disgruntled employee using malicious software – malware. Intentional destruction of data or network disruption can result from various forms of malware, including viruses, Trojan Horses (Trojans), spyware, worms, Ransomware, and rootkits. Organizations must provide at minimum annual security training so that the health information systems that the staff are using are not compromised (Conn, 2016). The appropriate password complexity and security must be enforced for each user of the system. The security precautions to prevent an internal breach include not sharing passwords and not downloading information or unauthorized software from insecure or forbidden sites.
The HHS (2019) provides security resources for healthcare organizations and providers. The first step is to create an organizational culture that is committed to HIPAA privacy and security requirements. It is important to perform a security risk analysis by reviewing policies, procedures, and staff activities as they relate to the HIPAA Security Rule, and then document the risk analysis processes. It is also important to develop an action plan that helps manage and mitigate the risks identified in the analysis.
Questions:
What legislation strengthened HIPAA security? Answer: The Health Information Technology for Economic and Clinical Health Act.
HITECH applied HIPAA security and privacy rule to whom? Answer: Business associates.
What are some of the threats to protected health information? Answer: Threats to protected health information include malware like viruses, Trojans, spyware, worms, ransomware, and rootkits.
How do hospitals and clinicians demonstrate the meaningful use of EHRs? Answer: To integrate clinical quality measures in patient care.
What are the HIPAA safeguards? Answer: Administrative, physical, and technical safeguards are used to secure an organization’s protected health data.
Electronic Health Records
The goals of the HITECH Act were to promote the adoption of EHRs since in 2008 only 10% of hospitals had adopted EHRs and the EHR allows access in real-time to patient information to authorized providers since it contains the medical history, diagnoses, medications, immunizations, and allergies of each patient. The certified EHR is a digital system that provides the most up to date data in the documentation of a patient’s medical information. When EHRs are integrated with clinical decision support tools, the provider is supported in their interpretation of the patient data that is currently available. This system can provide clinical reminders or alerts, aggregate the data into a central database for analysis, and provide a means of communication and collaboration with other providers and their patients through the patient portal. The EHR is interactive and can support complete documentation of a patient encounter through the use of the Computerized Provider Order Entry (CPOE) templates embedded in the EHR. The use of patient portals has improved communication between healthcare providers through the use of encrypted emails as well as access to the patient medical record. Access and accuracy of the information contained in the EHR is dependent upon messaging standards and terminology standards.
Technology and Standards for Healthcare
Messaging Standards
DICOM – Digital Imaging and Communications in Medicine (DICOM) developed for the transmission of images and used for Picture Archiving and Communication Systems (PACS).
IEEE – Institute of Electrical and Electronics Engineers (IEEE) sets standards for computers, computer languages, and medical instruments used at the bedside.
HISB – Health Information Standards Board (HISB) is a subgroup of the American National Standards Institute (ANSI) and provides an open forum for and coordination of healthcare informatics standards developing organizations.
HL7 – Health Level Seven (HL7) is an accredited ANSI standard organization that creates the messaging standards for healthcare information system interoperability to share electronic health information. Fast Healthcare Interoperability Resources (FHIR®) helps to define health data formats and elements by standardizing application programming interfaces (APIs) and supports the interoperability of legacy systems (HIMSS, 2021).
NCPDP – National Council for Prescription Drug Programs (NCPDP) founded in 1977 and helps make recommendations for the US National Drug Code with the vision of promoting healthcare standards and solutions related to pharmacy functions and HIPAA mandated transactions.
X12N – The Accredited Standards Committee (ASC X12) was chartered by the American National Standards Institute (ANSI) to develop and maintain the standards for Electronic Data Interchange (EDI) including business processes, financial data, healthcare, insurance, and HIPAA mandated transactions.
Terminology Standards
LOINC – Logical Observation: Identifiers, Names, and Codes (LOINC) is a coding system and database providing standards for medical laboratory observations supporting the electronic exchange of lab results.
Drugs – National Library of Medicine (NLM), Food and Drug Administration (FDA), and Veterans Administration (VA) collaborate on improving the interoperability of drug terminology with RxNorm that provides normalized names for clinical drugs and links this information to drug vocabularies and drug interaction software and the National Drug File Reference Terminology (NDF-RT) and are being added to the UMLS to represent clinical drugs.
Billing – Current Procedural Terminology (CPT) developed by the American Medical Association in 1966 and International Classification of Diseases, Tenth Revision (ICD-10).
Clinical – Unified Medical Language Systems (UMLS) was started in 1986 by the National Library of Medicine (NLM) to help distribute electronic knowledge sources where developers can enhance applications like digital libraries, natural language processing, and clinical decision support. The Systematized Nomenclature of Medicine Clinical Terms (SNOMED-CT®) is a combination of reference terminologies and clinical terms that is the standard for the electronic exchange of clinical health information and meets the requirements for interoperability between health information systems (NLM, 2021).
AHRQ (Agency for Healthcare Research and Quality, 2015) is the government agency that provides tools to help healthcare organizations by providing quality indicators and measures or metrics that are standardized based on their research on evidence-based health care. AHRQ has three types of metrics that help organizations assess the quality of care they are delivering: structural, process, and outcome measures. Structural measures evaluate the capacity, systems, and processes used by the health care provider to improve their provision of quality care. The process measures evaluate how effectively the healthcare provider follows the evidence-based clinical practice recommendations, meaning that the patients receive recommended preventive services. Finally, outcome measures assess the effectiveness of the health care services provided to patients and the response of the patients to those interventions. Medical or diagnostic errors can be prevented and reduced to improve patient safety. Errors can happen in any sector of the health care system: “hospital, clinic, surgery centers, doctor’s offices, nursing homes, pharmacies, and patient’s homes” (AHRQ, 2021b, para.1).
Benefits
The accuracy of data used in patient care and treatment is critical as a foundation for better clinical outcomes but also for accuracy in billing and timely reimbursements for healthcare services. The EHR design is to provide complete and accurate medical documentation on each patient. This data is accessed at the point of care, without the difficulties of reading an illegible paper record, and is critical for efficient and effective clinical decision-making. By sharing patient information outside of the healthcare organization or physician practice with other authorized healthcare providers, organizations are able to reduce the costs of duplicate testing, saving time and money for patients and providers. The coordination of care includes many stakeholders such as care teams and the patient in the management of the patient’s health. Streamlining administrative and business processes helps improve the value of these systems as well as increase patient safety and satisfaction.
Challenges
There are many challenges when adopting EHRs and CPOE. Some of the unintentional consequences when adopting these systems can be disrupted workflows that increase the clerical burden on the provider by including clerical documentation responsibilities in addition to the clinical documentation. The frequent changes to systems and user interfaces increase the disruption of work and learning curve included with each change. Some issues remain with using paper documentation since complex patient orders like Total Parenteral Nutrition (TPN) and Chemotherapy continue on paper orders because of the complexity and uniqueness of each order based on a specific patient’s needs. Although EHR and CPOE technologies change how medications are ordered, they can introduce new medication errors that result from confusing or overly complex graphical user interfaces where the CPOE can restrict medication orders and protocols that do not allow the clinician to order the appropriate medication because it is not an available selection (Herthog, 2010).
If the CPOE templates only offer the provider a check off box, a revision of the templates is indicated to provide more opportunities for specific documentation details. Providers and coders work in collaboration with the CPOE implementation team to make sure that the templates reflect best practice and billing requirements. Organizations must be aware that correcting one error – illegible handwriting, can create another – alert fatigue. Automating some processes like the medication interactions is very valuable as long as the pop-up alerts do not cause alert fatigue. The pop-up alert must be targeted and provide valuable information to the healthcare provider. If the alerts are frivolous, the provider is overwhelmed by the alert interruptions and can make errors by overriding all alerts because there are too many of them. For example, aspirin causes an alert with almost every drug, and it is a common prophylactic medication for stroke and heart attack. Alerts can be modified through the Pharmacy and Therapeutics (P&T) committee where pharmacists, clinicians, and physicians work together to assure their relevance in the practice setting. The configuration of CPOE templates can present a barrier to billing since accurate documentation is critical. Template configuration must allow the level of detail required to accurately meet the CMS code requirements for reimbursement of health services provided in patient care (CMS, 2021c).
Technology Literacy
As we see the usefulness of technology and recognize that adopting new technologies are disruptive, healthcare organizations should conduct a technology literacy assessment to identify training opportunities for the staff to reduce the resistance to change when moving from a paper-based medical record system to an electronic health record (Oo et al., 2021). The organization and staff need to identify areas of dissatisfaction with the current completeness and accuracy of medical documentation. Communication with the staff and providers helps them discuss their fears and concerns about the negative impact on their workflow, as well as recognizing the benefits a new EHR could provide. These discussions are most effective in open form venues where staff can share their experiences with working with these systems and reassure the skeptical staff that the improvements are worth the effort. This exercise also provides opportunities to identify staff as subject matter experts who are technology savvy and would be interested in supporting the EHR project planning, integration, and staff training. The usability and functionality of the EHR must be established before a healthcare organization considers their readiness for adopting the EHR and the future plan of joining a health information exchange.
The Triple Aim versus the Quadruple Aim
The Triple Aim for healthcare delivery that was proposed by the Institute of Healthcare Improvement in 2008 was focused on the improvement of patient outcomes by placing the patient at the center of care and to improve their experience when receiving care. The Quadruple Aim has been proposed resulting from the high rate of physician burnout that is reflected in a survey where between 68 percent of general practitioners and 73 percent of internists would not choose the same careers if they were able to make a different choice (Bodenheimer et al., 2014). As we consider the changes that have happened after the Triple Aim was introduced in 2008, ARRA mandated the adoption of the EHR, and in 2015 the ICD codes changed from ICD-9 to ICD-10 diagnosis codes where the number of codes have increased by five times (Cartwright, 2013). It is clear that the clerical burden has greatly increased for clinicians and the dissatisfactions they are feeling may be related to these changes. The Quadruple Aim considers that physician burnout has consequences for both the patient and physicians (West, 2016). West identifies the drivers of physician satisfaction as the effort, efficiency, work-life balance, control of work, and meaningful work. Bodenheimer et al. conclude that “positive engagement, rather than negative frustration” (2014, p. 575) is the key to improving population health.
Questions:
What must a certified EHR be integrated with to support the interpretation of current patient information by the healthcare provider? Answer: Clinical decision support tools help providers to correctly interpret patient information.
What is a primary benefit of using an EHR? Answer: The EHR is designed to provide complete and accurate medical documentation on a patient.
What is a major challenge introduced by medication alerts? Answer: Alert fatigue can result when healthcare providers are overwhelmed by too many frivolous alerts.
What is a major barrier when adopting new technologies? Answer: New technologies are disruptive and can lead to staff resistance and dissatisfaction if they do not have the technology literacy or needed training.
What is the triple aim and the quadruple aim? Answer: The triple aim places the patient at the center of care and improvement of the patient experience, the triple aim considers the high rate of physician burnout.
System Acquisition Project Management Institute Processes
As healthcare organizations adopt these new technologies to meet the requirements of legislation like ARRA, HITECH, and HIPAA, the system acquisition process is a key factor in conserving human and financial resources. One of the risks when adopting new technologies and information systems, aside from the cost, is the end-user acceptance of the new system as discussed in the section on technology literacy. There is a discussion on end-users as their subject matter experts in project planning later in this section. It does not matter if the project is the adoption of an EHR or if it is participation in a health information exchange (HIE), the risk of failure is very high – up to 29% as discussed by the Standish Group in their CHAOS Report (2015). Involving staff as subject matter experts is a good investment in the organization’s people, minimizes potential resistance to the implementation, and helps achieve most functionality needed the first time.
When an organization is preparing to select a new information system there are several factors involved in the planning of the new system. According to the Project Management Institute (2020), the first phase of a project is the initiation phase which is focused on making sure that the project will meet the business needs of the organization. So, the needs of the organization and the staff must be determined so that the new system aligns with the organization’s mission, vision, and strategic goals. This can be accomplished through a workflow analysis and sharing the vision of where the organization wants to be in the near future. Once the functionality the system needs to provide for the organization is determined, then the project management process begins. During the initiation phase, the project charter and project scope are created. The steering committee creates the project scope which is one of the most critical parts of a project found in the charter. This document explains the project goals and the tasks that will be accomplished during the project. The needed work is identified along with major milestones, the initial timeline, and the identification the internal and external stakeholders. The project manager is selected in the initiation phase. The CEO is often the project sponsor, and they control the resources available for the project.
The next phase is the project planning phase. The deliverables during this phase are the Work Breakdown Structure (WBS), a detailed project plan, a list of requirements, and a plan for communication. It is very important to understand exactly what work must be planned and this must be documented in detail. To accomplish the necessary details, it is very important to for the project team to meet and discuss the objectives of the project and determine what is needed to accomplish those objectives. A WBS must be very detailed so that each task is manageable and the deliverables are measurable. This part of the process can take time depending on how complex the project is. A change management process must be in place to prevent wasted resources and scope creep. Scope creep occurs when the project scope expands by adding features or functionality that was not included in the original scope identified in the project plan. This can result in increases in budget and human resource costs or increased time to complete the project. A change management process is needed so that requests for modifying the original scope are reviewed and approved or rejected. Communication with the project team helps in understanding the project plan, the project scope, and helps avoid unnecessary changes.
The request for information (RFI) and or the request for proposal (RFP) is the next step in this process. When soliciting vendors, it is important to research the potential vendors you may be interested in since a great deal of information is available on the Internet so the possibilities can be narrowed to a few vendors. Depending on the information that you receive from the vendors, it may be a good strategy to ask for a proof of concept where they demonstrate the effectiveness and ease of use of their system. It is a good strategy to avoid resistance from the staff since they will be able to visualize the system and then they can ask questions and the vendors can answer the questions that the staff may not have thought of previously. Having vendors demonstrate side-by-side lets everyone compare the systems.
Once the final system is selected, the execution phase can begin. The coordination of people and resources begins to accomplish the project work. Documentation will include minutes from the project team meetings and any additional record keeping that must be included. It is important that communication and updates are provided to the stakeholders and steering committee.
Project execution requires monitoring and controlling the project by tracking the completion of the work and milestones with careful documentation of the project progress and metrics used to support the quality required has been achieved. The appointed change agents must approve any changes to the project deliverables. This phase is very important to document and measure progress and communicate those findings, makes needed adjustments to provide the quality, budget requirements, and project on schedule. When closing a project, it is important to document any lessons learned during the process so that this information is available for future projects.
Delivering HIT value
The healthcare environment has changed a lot after adopting EHRs with CPOE to improve the quality of patient care. Important considerations when adopting these technologies are: 1) an experienced project management team, 2) subject matter experts – if those resources are not available inside the organization they must be hired, 3) proper identification of the stakeholders, 4) an IT staff that can support and maintain the systems, 5) an education and training staff to support organizational changes, and 6) development of physician champions to advise and support the changes. Quality outcomes are not simply a result of implementing technology but must result in improved patient outcomes by leveraging those new technologies. Planning is a critical component of successful implementations, and the clinical stakeholders need to be included in the planning and implementation stages.
Subject Matter Experts
If organizational leadership has the vision to use the end-users as their subject matter experts (SMEs), they can benefit from their expertise in the planning and implementation of the project, it allows the organization to create “super-users” that can train and support the staff after the system “goes live” and the formal training from the vendor has ended. Multidisciplinary teams are a critical contributor during the planning of these complex systems so that the functionality and usability of the new system is maximized. Including the department trainers as part of these teams are SMEs is a great strategy since they know what their department needs the information system to do to accomplish the daily work required to support the patients and clinical staff. The advantage of including these staff members as super-users is that they can support their departments after the system goes live and the formal training from the vendor has ended. It does not matter if the project is the EHR or if it is participation in an HIE. This strategy a good investment in the organization’s people and it avoids potential resistance to the implementation, but it also helps the organization get most of the functionality right the first time.
Questions:
What is the key factor in system acquisition? Answer: The key consideration is system acquisition is the conservation of human and financial resources.
What report discussed the high risk of EHR adoption failure? Answer: The CHAOS Report provided the Standish group sited that up to 29% of EHR adoptions fail.
What is the importance of the project scope? Answer: The project scope explains the project goals and the tasks that will be accomplished during the project.
What is the measure of that quality outcomes have been achieved? Answer: The achievement of quality outcomes is demonstrated by improved patient outcomes.
What is the value of super-users? Answer: The super-user can support the departments after the system goes live and the formal training has ended.
Application of Technology in the EHR
Incorporating innovative technologies with health information systems is important in achieving the patient safety goals expressed in the IOM studies. The use of electronic health records includes the use of computerized provider order entry (CPOE), Clinical decision support systems (CDSS) that include E-prescribing, medication administration that includes bar-code medication administration (BCMA), smart pumps, and automated medication dispensing cabinets (ADC). The use of electronic medication administration record (eMAR) software and patient data management systems (PDMS) help support clinical documentation at the bedside. Patient portals have provided patients with access to their medical records, the ability to schedule appointments online, pay their bills, and communicate with their healthcare providers.
Computerized Provider Order Entry
CPOE, an initiative coupled with the EHR adoption within the HITECH Act that was made law in 2009 within the American Recovery and Reinvestment Act (ARRA) to address the handwriting issues. Incentives were offered to healthcare organizations and eligible professionals to encourage them to adopt EHRs. The introduction of technology has solved some of the medical errors related to handwriting and documentation issues, but had introduced workflow disruptions, template configuration issues, and pop-up alerts that break the providers concentration and can result in technology initiated errors. The use of CPOE templates help streamline the provider’s selection process during order entry. The issue is if the templates are not correctly designed, they are not fully usable. Checklists and flowcharts can be applied to CPOE templates and it is very important that the clinical staff that will be using those templates are involved in the planning and design so that the details are complete and correct. The ability to copy and paste notes, known as cloning, is a feature that is disabled in CPOE templates since without a correct assessment of patient, errors could be introduced and the wrong treatment could result.
Clinical Decision Support Systems
The Centers for Medicare and Medicaid Services provided a tip sheet to help healthcare organizations understand clinical decision support system (CDSS) tools. The functionality of CDS systems is available on a variety of platforms such as the EHR, patient portals, mobile devices, and cloud service providers. These tools are intended to support the healthcare team in making high quality informed care decisions at the point of care. The “CDS Five Rights:” 1. right information, 2. right people, 3. right channels, 4. right intervention formats, 5. rights points in workflow (CMS.gov, 2014). The right information is dependent on evidence-based guidelines and supports clinical decision-making at the point of care. The right people include the care team and the patient in partnership with them. The patient must be engaged in the decision-making about their care as recommended by the Centers for Disease Control and Prevention (2021) as there is evidence that engaged patients have greater knowledge, skills, and confidence that help improve health literacy and disease outcomes. The right channels include the EHR, patient portals, mobile devices, and cloud service providers allowing improved access and communication for the care team and the patient. The right intervention format includes alerts, order sets, CPOE templates, flow sheets, patient monitoring systems, and dashboards that provide information at a glance for administrators and clinicians. Finally, the CDSS must be available at the right point in the workflow to best support clinical decision-making and interventions.
Medication Administration
Bar-code medication administration works in tandem with the electronic medication administration record (eMAR) and is helpful for the nursing staff to comply with the “Five Rights” of medication administration: the right patient, right dose, right route, right time, and right medication (AHRQ, 2021b; Hanson, et al.,2021). Smart infusion pumps have been adopted since they have safety features that include the detection of air within the intravenous line and have a battery backup in the event of a power failure so that the administration of medication by infusion is continued. The use of infusion pumps provide better control over manual medication infusions since uncontrolled infusion can result in patient harm or death (Shah, et al., 2020). Automated medication dispensing cabinets (ADC) are widely used in the United States and provide secure access to medications while improving the management of controlled/narcotic medications (Craswell, et al., 2020). Patient data management systems (PDMS) are important systems that help compile multiple sources of data that is gathered from vital sign monitors, other medical devices such as ventilators, laboratory results, and medical imaging (Dupont, et al., 2019). These systems help increase medication safety and reduce medication errors.
Questions:
What helps streamline the provider’s selection process during order entry? Answer: The CPOE template helps streamline order entry.
What is cloning? Answer: Cloning is the ability to copy and paste patient notes in an EHR.
What are the CDS five rights? Answer: The right information, the right people, the right channels, the right intervention formats, and the right points in the workflow.
What are the five rights of medication administration? Answer: The right patient, right dose, right route, right time, and the right medication.
What technologies are used to administer medications to patients safely? Answer: The use of technology to administer medication can be the use of bar-code medication linked with the eMAR, smart infusion pumps, and automated medication dispensing cabinets.
Patient Engagement Technologies and Services
Patient engagement is important to support the best patient outcomes and partnerships with their primary care provider. The adoption of EHRs has provided access to a patient’s medical information through the patient portal. The patient portal is an important communication tool where the patient can view their medical record, lab results, pay invoices, but most importantly, it is a tool to support encrypted emails through unique usernames and passwords. This information is available at all times (24/7).
One concern for patient engagement is that the older adults may have several challenges when using the patient portal or telehealth technologies if they are unfamiliar with computers or do not have technology literacy. This presents a barrier since this aging population often has chronic illnesses and comorbidities that can not only affect their quality of life but may worsen due to the lack of physician monitoring and oversight. According to the study by Doraiswamy, et al. (2021), older people were affected by COVID-19 disproportionally when compared to other groups since they are more vulnerable to respiratory complications and has been a leading health complication during the pandemic. There is an opportunity to improve access to telehealth services for the older adults and we need to determine how the usability of these hybrid models of care can be increased for this vulnerable patient group.
Patient Engagement and Social Determinants of Health
The Social Determinants of Health (SDoH) are often at the root of health inequities, and we saw these disparities increase during the COVID-19 pandemic and highlights there is a lot of room for improvement in our healthcare system. The SDoH is composed of several patient demographics and environmental domains: economic stability, education, access to health services, the physical environment the patient lives in as well as the social and community context (HealthyPeople, 2022). The additional factors that we must consider for patients is that they may have difficulties with Internet access or limited digital literacy as a result of SDoH. According to Chang et al. (2021, p. 343) over one third of households headed by people over 65 years old do not have access to a computer and over half do not have a smartphone. One of the most promising innovations that we have is the potential to improve patient health literacy using smartphones and mHealth. The mHealth barriers to smartphone ownership were the factors of age, male, less educated, and lower annual income. These patients might be excluded from using mHealth interventions (Bommakanti et al, 2020). It is important for communities and healthcare organizations to consider how to overcome these barriers.
Telehealth and Telemedicine
During the COVID-19 pandemic, there was wide adoption of telehealth and telemedicine to provide healthcare to patients while keeping them safe. Telemedicine uses telecommunication technologies like your computer, tablet, or smartphone over the Internet to let you talk to your doctor live either by phone or video chat (Chiron Health, 2022). Telemedicine uses electronic communications and software to provide clinical services without the need for an in-person visit in the doctor’s office. Telemedicine supports remote monitoring so your doctor and review any changes you are experiencing from home (Chiron Health, 2022). Telehealth provides non-clinical services such as provider training, medical education, and support the ability to send and receive secure messages and exchange files with your healthcare provider (HHS, 2022).
Although telemedicine / telehealth may seem to be an entirely new technology, it really is not. NASA pioneered telemetry and telemedical technologies to use in the space program to monitor the life signs of the astronauts. There is benefit in the application of this communication technology to support rural populations that are often medically underserved. An application of virtual health care visits as well as remote monitoring capabilities is the current opportunity in using these emerging technologies. The only way that many patients were provided continuity of care when in-person visits were restricted was to the virtual visit using telehealth platforms (Bird, 2021). The financial savings of using telehealth technologies are very promising. Another advantage is to expand access to specialists to support patient care when these specialists are unavailable at the local level. Information technology infrastructure is inadequate, especially in rural locations.
Telehealth can take the form of audio and video (synchronous), store-and-forward technologies (asynchronous), and remote patient monitoring (internet and communication technology (ICT) (Rangachari et al., 2021). Providing safe and efficient care to patients has always been the goal of healthcare and pre-COVID-19 the use of telehealth was restricted due to policies governing telehealth services that will be covered and reimbursed. Currently State laws and Federal regulations are being considered since there are licensing and reimbursement barriers that may prevent the level of the use of telehealth technologies (Lewis, 2021; Maheu, 2021). During the pandemic, there was a temporary change that removed the licensing and reimbursement restrictions. We want to explore the sustainability of telehealth as a treatment option for the wide range of patient groups and it’s utility as a communication tool (Doraiswamy et al., 2021; Graham et al., 2021; Lieneck et al., 2021; Nicosia et al., 2021; Purnell et al., 2021).
Telehealth Modalities
Several telehealth modalities allow healthcare personnel and patients to connect using technology to deliver health care:
Synchronous: This includes real-time telephone or live audio-video interaction typically with a patient using a smartphone, tablet, or computer. In some cases, peripheral medical equipment (e.g., digital stethoscopes, otoscopes, ultrasounds) can be used by another health care provider (e.g., nurse, medical assistant) physically with the patient, while the consulting medical provider conducts a remote evaluation.
Asynchronous: This includes “store and forward” technology where messages, images, or data are collected at one point in time and interpreted or responded to later. Patient portals can facilitate this type of communication between provider and patient through secure messaging.
Remote patient monitoring: This allows direct transmission of a patient’s clinical measurements from a distance using cloud technologies (may or may not be in real time) to their healthcare provider.
There are many benefits to the applications of telehealth that include TeleSleep (Nicosia et al., 2021), TeleSurgery (Purnell et al., 2021), outpatient patient-provider video conferencing (Lieneck et al., 2021), mental health support services (Zimmerman et al., 2021), virtual physical exam guidelines (Benziger et al., 2021), and maternity support (Westwood, 2021).
Remote Monitoring
As the use of remote diagnostic monitoring devices and sensors increases, access to the cloud is needed to communicate information to the healthcare Internet of Things (IoT). The IoT is now part of the healthcare architecture made up of the perception layer, network layer, and application layer (Kelly et al., 2020). The perception layer of the IoT architecture would sense the data to be collected. Sensing systems that collect data include radio frequency identification (RFID), GPS, and smart devices are capable of sending digital information so the healthcare provider can monitor the results in real time. This would allow faster treatment or intervention if the values were out of range. It is important to understand that not all devices are clinically tested for safety or effectiveness. The network layer would include both wired and wireless networks including Bluetooth, and wireless telecommunication networks. The application layer applies artificial intelligence (AI) which is capable of performing image analysis, text and language recognition giving the ability to compare a patient’s past results with the current data available through the application layer. As healthcare moves in the direction of eHealth that is Internet based delivery of health services and policies are required to develop the IoT infrastructure and implementation.
Devices
There are many varieties of remote patient monitoring devices that include: continuous glucose monitor, anticoagulation testing, electrocardiography devices, heart rate monitors, medical alert systems, maternity care monitoring, pediatric monitoring, pulse oximeter, smart scale, medication monitoring, and patient wearables (Welkin Health, 2020). Devices such as smartphones and computers allow easy access to a remote healthcare provider through virtual visits from the comfort of their home. Many new technologies such as blood pressure cuffs, glucose meters, and pulse oximeters can upload data for the provider. Remote monitoring is a useful tool to provide the healthcare provider with accurate measures of the patient health, but also allows the older adult to age in place with less travel and exposure to communicable diseases like COVID-19. According to Zimmerman et al. (2021) a patient satisfaction survey was conducted to compare in-person versus virtual mental health visits. These visits were five days a week in an intensive setting and could be as long as six hours a day. The overall satisfaction of this treatment was high; however, many patients were more satisfied with the interpersonal group setting when it was in person. Finally, older patients were at risk of not having access telehealth services until Medicare allowed the Medicare Part B beneficiaries telehealth access while the pandemic lasts (Custer, 2020).
One of the challenges when conducting a virtual visit is the communication between the physician and the patient is complete so that a proper patient assessment can be achieved. Benziger et al. (2020) made the following recommendations based on their findings: accurate measurement of vital signs is made with a validated digital blood pressure cuff that also measures the heart rate, an accurate electronic weight scale, oxygen saturation, and temperature measurements are needed. If needed, a skin assessment that reports any new bruises, rashes, or swelling can be done visually. An assessment of the head, eyes, ears, nose, and throat is important especially if there are any changes. Any neck pain, wheezing, tachypnea, shortness of breath should be reported. Patients can be asked to turn their heads for example. Pulse and other heart indicators can be measured with wearable devices. Assess any abdomen changes: firm, tender, or distended. Assess edema in the extremities. Take note of any neurological changes in speech, gait, and the ability to stand from a seated position. Finally, the social determinants of health such as diet, physical activity, sleep, stress, housing, transportation, safety, and mood should all be assessed.
Questions:
What are the Social Determinants of Health? Answer: SDoHs are economic stability, education, access to health services, physical environment, and community environment.
Why is patient engagement important? Answer: The value of patient engagement is the formation of partnerships between patients and their providers that result in better patient outcomes.
What is the benefit of leveraging technology for patient care? Answer: The benefits of leveraging technology in patient care are increased access to care, enhanced communication between patients and providers, and improved quality of life and health outcomes.
What are the challenges in leveraging technology for patient care? Answer: The Social Determinants of Health, technology literacy, access to smartphones, and the internet are all barriers to patient care.
What technologies are used to support remote access to care? Answer: The use of telehealth for many health services such as virtual office visits, mental health support, and remote monitoring devices to communicate patient data for provider monitoring.
Health Information Exchange (HIE)
The HIE supports the sharing of electronic health data between two or more healthcare organizations or providers. The HIE can also be an organization that provides this technology at a local, state, regional, or national level that provides a secure ability to share health data. The STAR (Strengthening the Technical Advancement & Readiness of Public Health via Health Information Exchange) Program expands the ability of HIEs to support public health agencies in response to health emergencies and pandemics such as COVID-19 (HealthIT, 2021b). The HIE is a hub of data that is pulled from multiple sources that can include local communities, regional, and state entities and depend on policies that define how data can be used in public health agencies. Original participants in the STAR HIE program include Georgia Health Information Network, Health Current Arizona, Kansas health Information Network, HealthShare Exchange of Southeastern Pennsylvania, Inc., and Texas Health Services Authority (HealthIT, 2021b).
The Trusted Exchange Framework (TEF) is the result of the 21st Century Cures Act that created the following principles for interoperability: 1) standardization of technical components, policies, best practices, and procedures, 2) openness and transparency of activities, 3) cooperation and non-discrimination, 4) privacy, security, and safety, 5) authorized access to digital health information, and 6) equity, and 7) public health to develop a learning health system to improve population health and lower the cost of care (HealthIT.gov, 2024).
There are several types of Health Information Exchanges (HIEs) we must be aware of:
Hybrid HIEs support the collaboration between healthcare organizations and include Patient Centered Medical Homes (PCMHs), Accountable Care Organizations (ACOs), and vendors in specific service regions (HIMSS, 2021).
Proprietary HIEs that are private, located in a community or network that are often based in a single organization that provides the oversight of the aggregation of patient data into a centralized database (HIMSS, 2021).
Regional HIEs are inter-organizational and usually they are not-for-profit and require a variety of funding sources (HIMSS, 2021).
State-wide HIEs are a broader approach where the exchange of patient information between organizations is often coordinated through technical workgroups such as HITOC (Health Information Technology Oversight Council, 2021) in Oregon in efforts to coordinate and reduce the cost of care for their population.
The directed exchange is an HIE where the patient information can be securely sent between healthcare providers allowing the coordinated care of the patient (HealthIT, 2021c).
The query-based exchange where a request for health information on a specific patient from a different healthcare provider that is working to give unplanned care (HealthIT, 2021c).
The consumer mediated exchange helps the patients have the ability to aggregate and have complete control of the release and use of their health information (HealthIT, 2021c).
One of challenges of the HIE is the need for a master patient index that provides unique identifiers so that the patient information is unique to that patient and not merged with a patient who has the same name. The capability of keeping correct patient information is used at an organizational level with medical record numbers associated with unique patients. The danger of incorrect treatments based on incorrect patient information can happen when sharing patient information outside the organization. This is one reason that patient engagement in their care and review of the documentation in their medical record is so important.
Questions:
What program expands the ability of HIEs to support public health agencies in response to health emergencies and pandemics? Answer: The STAR (Strengthening the Technical Advancement & Readiness of Public Health via Health Information Exchange) Program.
What is one of the greatest challenges in implementing an HIE? Answer: The master patient index that provides unique identifiers for specific patients has not been developed.
What type of exchange help patients have the ability to aggregate and have complete control of the release and use of their health information? Answer: The consumer mediated exchange.
What type of HIE is where the patient information can be securely sent between healthcare providers allowing the coordinated care of the patient? Answer: The Directed Exchange.
What type of HIE is private and is located in a community or network that are often based in a single organization that aggregates patient data into a centralized database? Answer: The proprietary HIE.
Future of Health Information Technology
The COVID-19 pandemic demonstrated the need for healthcare providers to adopt EHRs and other digital technologies like telehealth and HIEs to expand access to care for all patients. The need to adopt EHR technologies will increase the focus on the standardization that results in the consistency of formats, accuracy of data, interoperability through data standards and protocols for better care coordination and clinical decision-making, and the streamlining of processes that improve workflow efficiency and productivity (Evident, 2023). Improvements in securing patient information in the future may use new technologies like blockchain (Ahmad et al., 2021). Blockchain is a digital ledger of trusted transactions and is likely an important component of the next generation Internet – the Decentralized Web or Web 3 (Walkweltech, 2019) and is a distributed database that stores encrypted transaction records. Since blockchain is a public file there is no audit trail and currently since HIPAA requires the audit trail to be visible regarding PHI, blockchain in its current form is not HIPAA compliant, but could be developed to accommodate that requirement.
5Vs of Big Data Analytics
Due to the huge amounts of complex medical data being collected in EHRs through lab values from tests, diagnostic imaging, sensor devices, and genomics. This large amount of complex data requires an analysis strategy so that it is useful and creates actionable information. The characteristics of big data are “value, volume, velocity, variety, veracity, and variability” (Ristevski & Chen, 2018, p. 2). The sheer volume of medical and health related data is increasing exponentially, and the velocity refers to the speed and amount of data created. The variety of the data depends on if the data is structured, unstructured, or semi-structured. The veracity of the data means what relevance, reliability, quality, and predictive value the data may provide. Data variability considers if the data is consistent over time. Finally, the value of the data is when it is analyzed that it provides value to the patients and clinicians who will use it. Big data analytics has the potential of improving patient care by detecting diseases and trends more quickly to reveal patterns of disease and providing actionable knowledge to healthcare providers and public health. If data points are missing this can change the analysis and lead to erroneous conclusions. There are also privacy and security issues with the use of big data in healthcare since medical data is sensitive and must be kept confidential. Encryption and the de-identification of the data is needed so that personal information is not accidentally revealed.
Artificial Intelligence
Artificial Intelligence (AI) and Machine Learning (ML) are opportunities that we will be applying to the large amounts of patient data that is generated everyday (Fernandez, 2018). Artificial Intelligence is a predictive algorithm that helps model and analyze diagnostic images, generate clinical documentation, and support clinical decision-making. The application of AI to digital diagnostic imaging is a critical opportunity for streamlining the diagnosis of disease and can help identify disease trends in different geographic locations. ML is a type of AI where the algorithms developed are based on computational statistics. This data can “teach” the computer by recognizing patterns in the data, the larger the dataset provided, the more precise the output will become. COVID-19 demonstrated the value of predictive analytics that helped medical providers to respond to the trends and spread of the disease to support population health and improve patient outcomes. Although AI and ML are powerful tools, they are only as good as their programming and the dataset diversity used to train the algorithm. If incomplete datasets are used to train AI and ML, bias can be introduced by including existing prejudices around race or gender for example. Addressing this ethical concern means that these programs must be free of errors. Human oversight is needed since AI and ML systems are not infallible (Juneja, 2022).
AI Transparency Rule
The Department of Health and Human Services released the Health Data, Technology, and Interoperability: Certification Program Updates, Algorithm Transparency, and Information Sharing (HTI-1) Final Rule (HealthIT, 2024b) in December of 2023 to implement provisions of the 21st Century Cures Act and update the ONC Health IT Certification Program. This rule requires the AI developers to provide healthcare organizations with the information they need to evaluate the fairness, validity, appropriateness, effectiveness, safety by understanding the algorithm’s intended role in clinical decision-making, and the cautions that must be observed when using the AI. The source of the datasets used in training the AI and performance metrics must be disclosed to the customers by the developers of these technologies. As more AI technologies are applied to healthcare systems, they must meet the ethical standards of responsible analysis that is evidence-based, free of bias, and promotes health equity (Diaz, 2023).
HTI-1 Final Rule (HealthIT, 2024b)
Algorithm Transparency: Establishes first of its kind transparency requirements for the artificial intelligence (AI) and other predictive algorithms that are part of certified health IT. ONC-certified health IT supports the care delivered by more than 96% of hospitals and 78% of office-based physicians around the country. HHS’ leading-edge regulatory approach will promote responsible AI and make it possible for clinical users to access a consistent, baseline set of information about the algorithms they use to support their decision making and to assess such algorithms for fairness, appropriateness, validity, effectiveness, and safety.
USCDI Version 3: Adopts the United States Core Data for Interoperability (USCDI) Version 3 (v3) as the new baseline standard within the ONC Health IT Certification Program (Certification Program) as of January 1, 2026. Developers of certified health IT will also have the ability to move to USCDI v3 sooner. USCDI v3 includes updates to prior USCDI versions focused on advancing more accurate and complete patient characteristics data that could help promote equity, reduce disparities, and support public health data interoperability.
Enhanced Information Blocking Requirements: Revises certain information blocking definitions and exceptions to support information sharing, and adds a new exception to encourage secure, efficient, standards-based exchange of electronic health information under the Trusted Exchange Framework and Common AgreementSM (TEFCASM).
New Interoperability-Focused Reporting Metrics for Certified Health IT: Implements the 21st Century Cures Act’s requirement to adopt a Condition of Certification (the “Insights Condition”) for developers of certified health IT to report certain metrics as part of their participation in the Certification Program. These metrics will give more insight into how certified health IT is used in support of care delivery.
Cloud Technologies in Healthcare
Cloud services are very cost-effective since they are highly scalable and offer a variety of services to healthcare organizations: Infrastructure as a Service (IaaS), Platform as a Service (PaaS), and Software as a Service (SaaS) (Oh et al., 2019). The cloud platform offers healthcare organizations and providers the ability to personalize the services that they need. Mobile internet and communication technology (ICT) provides a network for wearable technologies like biomedical sensors that provide the ability to remotely monitor a patient and connect these devices including the Internet of Medical Things (IoMT). Securing information in the cloud will likely include the use of blockchain technologies (Xu et al., 2022) and the use of multifactor authentication (Fakroon et al., 2020).
Internet of Medical Things
The Internet of Medical Things (IoMT) connects many devices that are widely distributed. The opportunity to leverage wearable devices to help patients and their care providers manage chronic disease through remote patient monitoring cannot be overlooked. The interoperability and connectivity of healthcare devices depends on how the device communicates its data such as a one-way transmission of data to the provider. Integrating data from different devices provides a better understanding of the patient and their current conditions. Patient engagement and understanding about using medical devices will provide the benefit of better patient outcomes through early detection and interventions by their provider. Botta et al. (2016) suggest that the Cloud and IoMT must integrate radio frequency identification (RFID) technology, wireless sensor networks, and smart devices that are capable of sending digital information. Cloud computing is a layered architecture composed of the hardware, storage infrastructure, platform composed of the software framework, and web service applications (Botta et al., 2016). The IoMT is being used to support eHealth where data is stored in the cloud and shared (Kelly et al., 2020). The security, privacy, and confidentiality factors of these new technologies like the IoMT, Cloud computing, and remote monitoring will be a challenge in meeting HIPAA requirements since these technologies are currently vulnerable to cyberattack.
PixelCrayons. (2022). Cloud Computing in Healthcare: The Pros and Cons. Retrieved from https://www.youtube.com/watch?v=xEl_6NZuyS4
Robotic Process Automation
Robotic Process Automation (RPA) is a technology that extracts data, fills in forms, and moves files. This software helps to automate repetitive tasks and can expand the use of AI and ML, natural language processing, and computer vision (IBM, 2020). The difference between AI and RPA is that AI is data-driven and RPA is process-driven. The RPA processes are defined by end-users. RPA has the potential to digitize work by automating repetitive processes to improve organizational performance (Ratia et al., 2023).
Cybersecurity
Cybersecurity and data privacy are ongoing concerns as the adoption and use of these innovative technologies increase. HIPAA compliance is provided by most telehealth video conferencing platforms. Encryption is an important step needed to protect private data during the use of video conference calls and IoMT devices (Softermii, 2022). Although the IoMT and cloud computing provide many opportunities to share patient information and data, the information is vulnerable since cloud service providers are not covered entities. This means that they do not have to follow HIPAA regulations and organizations must use business associate agreements and encryption to protect the PHI. As always, we must formulate our policies around the security and privacy rules.
Two-factor authentication is needed to confirm the identity of a user on a system so that the confidentiality and privacy of patient information is preserved. Security is very important for preserving the integrity in access and transmission of that data. One method for biosensor devices is to use the Physically Unclonable Function that creates a secret key and stores it. Devices must be enrolled by the manufacturer by assigning a unique ID and set of challenge-response pairs (CRP) and a secret key that is associated with each CRP (Fakroon et al., 2020). Another security authentication measure in an organization is a password and a biometric that the individual possesses like a fingerprint. This is accomplished by the biometric data being captured, a signal process that stores the distinguishing feature from the biometric sample, reference templates are stored on a server or client, matching system that compares the biometric sample to the template, and then a decision system that verifies the match or rejects it because there is not a match (Bhargav-Spantzel et al., 2007).
Blockchain security is a distributed ledger technology (DLT) in a peer-to-peer network environment. Blockchain can be public where no permissions are required, private that require permissions, and consortium blockchains are run by organizations. The advantages of public blockchain are that they are independent from any organization but the network is slower. The advantages of using private blockchain is that there is access control by the organization. and improved performance, but it cannot be audited. The consortium blockchain supports data privacy such as elliptic curve cryptosystems (Campbell, 2023; Kim et al., 2020; Xu, 2022).
Questions:
What is a distributed digital ledger? Answer: Blockchain.
What characteristics are described by value, volume, velocity, veracity, and variability? Answer: The 5Vs of big data.
What can incomplete datasets used to train artificial intelligence algorithms cause? Answer: Bias in the assessment of data.
What technology integrates with medical devices using cloud architecture? Answer: The Internet of Medical Things.
What concerns do people have with using cloud technologies? Answer: Data privacy and cybersecurity.
Conclusions
The history of health information technology grew out of the need for accurate patient documentation so that information is available at the point of care so the most informed clinical decisions can be made. Healthcare information systems (HIS) have become more complex as a result. HIS includes laboratory, pharmacy, diagnostic imaging, and remote monitoring devices that all contribute data to the EHR and clinical decision support systems.
Patient information shared by using the Internet requires that healthcare organizations comply with the legislation designed to protect health information such as HIPAA and HITECH. Computer and technology literacy can create difficulties for the end-users unfamiliar or uncomfortable with those systems. However, with leadership that supports the participation of the staff in the system planning and implementation they can contribute their insights to achieve the system functionality and usability needed to do daily work and meet the organization’s mission, vision, and strategic goals. The interoperability of health information systems prepares the organization to participate in a health information exchange to expand a patient’s access to care. Emerging technologies like telehealth and remote monitoring devices will further improve the experience and benefits of technology to improve their health.
Key Words
Caregiver. A person who provides help to an individual who requires assistance with daily living due to old age, disease, a mental disorder, or disability. Caregivers can be paid, but are often unpaid family members or other persons from the individual’s social network. Typical tasks of caregivers include helping the individual to eat, bathe, dress, and use the toilet, as well as pay bills, clean the house, manage medicine, and monitor health. Caregiving can be highly stressful for caregivers, especially when caring for someone who is severely disabled or suffers from mental problems.
Disparities. Healthcare disparities are differences in access to or availability of medical facilities and services and variation in rates of disease occurrence and disabilities between population groups defined by socioeconomic characteristics such as age, ethnicity, economic resources, or gender and populations identified geographically.
Life Expectancy. Actuarial determination of how long, on average, a person of a certain age is likely to live.
Paraprofessionals. Personnel, such as certified nursing assistants and therapy aides, who provide basic assistance with activities of daily living and/or assist licensed and professional staff.
Home Health. A wide range of health care services that can are provided in the home for an illness or injury. Services include nursing, therapy, and health-related homemaker and social services.
Home Care. Help with daily activities to allow people to stay at home. Home care is sometimes called personal care, companion care, custodial care or homemaker services.
Functional limitation. The restriction or lack of ability to perform an action or activity in the manner or within the range considered normal that results from impairment. Usually applies when an individual does not have the physical, cognitive or psychological ability to independently perform the routine activities of daily living.
Cognitively impaired. When a person has trouble remembering, learning new things, concentrating, or making decisions that affect their everyday life.
Rehabilitation. A set of interventions /therapies that restore lost functioning or optimize functioning and reduce disability in individuals with health conditions.
The Joint Commission. An independent, not-for-profit organization, previously called the Joint Commission on Accreditation of Healthcare Organizations (JACHO), that sets standards and accredits healthcare facilities.
Hospice. Services that focus on the care, comfort, and quality of life of a person with a serious illness who is approaching the end of life. Services include a blend of medical, spiritual, legal, financial, and family support. Services can be provided in a specialized facility, a nursing home or the patient’s own home.
Palliative Care. Specialized medical care for people living with a serious illness. This type of care is focused on providing relief from the symptoms and stress of the illness and can include curative treatment. The goal is to improve quality of life for both the patient and the family.
Advanced Directives. A legal document that states a person’s wishes about receiving or withdrawing medical care if that person is no longer able to make medical decisions because of a serious illness or injury.
Telehealth. The use of digital information and communication technologies, such as computers and mobile devices, to access health care services remotely, to support long-distance clinical health care, patient and professional health-related education, public health and health administration.
AI (Artificial Intelligence). AI is a wide-ranging branch of computer science concerned with building smart machines capable of performing tasks that typically require human intelligence.
References
AMCP (Academy of Managed Care Pharmacy). (2021). Health information technology organizations. Retrieved from https://www.amcp.org/health-information-technology-organizations
AHIMA (American Health Information Management Association). (2021). AHIMA history. Retrieved from https://bok.ahima.org/doc?oid=58133
Ahmad, R. W., Salah, K., Jayaraman, R., Yaqoob, I., Ellahham, S., & Omar, M. (2021). The role of blockchain technology in telehealth and telemedicine. International Journal of Medical Informatics, 148, 104399. https://doi.org/10.1016/j.ijmedinf.2021.104399
AHRQ (Agency for Healthcare Research and Quality). (2015). Types of health care quality measures. Content last reviewed July 2015. Agency for Healthcare Research and Quality, Rockville, MD. https://www.ahrq.gov/talkingquality/measures/types.html
AHRQ (Agency for Healthcare Research and Quality). (2021a). Bar-coded medication administration. Retrieved from https://digital.ahrq.gov/bar-coded-medication-administration
AHRQ (Agency for Healthcare Research and Quality). (2021b). Medical errors. Retrieved from https://www.ahrq.gov/topics/medical-errors.html
American Recovery and Reinvestment Act (ARRA) of 2009, 155 C.F.R. 111.5 (2009).
ANSI (American National Standards Institute). (2022). Retrieved from https://ansi.org/
ASPE (Assistant Secretary for Planning and Evaluation). (n.d.). Standards organizations for the NHII. Retrieved from https://aspe.hhs.gov/standards-organizations-nhii
Benziger, C. P., Huffman, M. D., Sweis, R. N., & Stone, N. J. (2021). The telehealth ten: A guide for a patient-assisted virtual physical examination. The American Journal of Medicine, 134(1), 48–51. https://doi.org/10.1016/j.amjmed.2020.06.015
Bhargav-Spantzel, A., Squicciarini, A. C., Modi, S., Young, M., Bertino, E., & Elliott, S. J. (2007). Privacy preserving multi-factor authentication with biometrics. Journal of Computer Security, 15(5), 529-560. https://doi.org/10.3233/JCS-2007-15503
Bird, H. (2021). A now-or-never moment for telehealth? HFM (Healthcare Financial Management), 75(4), 20–24. Retrieved from https://www.hfma.org/topics/hfm/2021/may/now-or-never-moment-telehealth-demand-remains-strong-technology-healthcare-industry.html
Bjelica, A. (2017). A short journey through the history of medical ethics. Medicinski Pregled / Medical Review, 70(3/4), 119–122. https://doi.org/10.2298/MPNS1704119B
Bodenheimer, T., & Sinsky, C. (2014). From triple to quadruple aim: Care of the patient requires care of the provider. Annals of family medicine, 12(6), 573–576. https://doi.org/10.1370/afm.1713
Bommakanti, K. K., Smith, L. L., Liu, L., Do, D., Cuevas-Mota, J., Collins, K., Munoz, F., Rodwell, T. C., & Garfein, R. S. (2020). Requiring smartphone ownership for mHealth interventions: who could be left out? BMC Public Health, 20(1), 1–9. https://doi.org/10.1186/s12889-019-7892-9
Botta, A., de Donato, W., Persico, V., & Pescapé, A. (2016). Integration of cloud computing and Internet of Things: A survey. Future Generation Computer Systems, 56, 684–700. https://doi.org/10.1016/j.future.2015.09.021
Brotman, J. J., & Kotloff, R. M. (2021). Providing outpatient telehealth services in the United States: Before and during coronavirus disease 2019. Chest, 159(4), 1548–1558. https://doi.org/10.1016/j.chest.2020.11.020
Burke T. (2010). The health information technology provisions in the American Recovery and Reinvestment Act of 2009: implications for public health policy and practice. Public health reports (Washington, D.C. : 1974), 125(1), 141–145. https://doi.org/10.1177/003335491012500119
Campbell, C. (2023). What are the 4 different types of blockchain technology? Retrieved from https://www.techtarget.com/searchcio/feature/What-are-the-4-different-types-of-blockchain-technology
Cartwright D. J. (2013). ICD-9-CM to ICD-10-CM Codes: What? Why? How?. Advances in wound care, 2(10), 588–592. https://doi.org/10.1089/wound.2013.0478
CDC (Centers for Disease Control and Prevention). (2018). Health Insurance Portability and Accountability Act. Retrieved from https://www.cdc.gov/phlp/publications/topic/hipaa.html
CDC. (2021). Patient engagement. Retrieved from https://www.cdc.gov/healthliteracy/researchevaluate/patient-engage.html
Choi, J., Jenkins, M. L., Cimino, J. J., White, T. M., & Bakken, S. (2005). Toward semantic interoperability in home health care: Formally representing OASIS items for integration into a concept-oriented terminology. Journal of the American Medical Informatics Association, 12(4), 410. https://doi.org/10.1197/jamia.M1786
Chiron Health. (2022). What is telemedicine? Retrieved from https://chironhealth.com/telemedicine/what-is-telemedicine/
CMS (Centers for Medicare & Medicaid Services). (2010). Medicare & Medicaid EHR incentive program. Retrieved from https://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/Downloads/MU_Stage1_ReqOverview.pdf
CMS (Centers for Medicare & Medicaid Services). (2014). Clinical decision support tipsheet. Retrieved from http://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/Downloads/ClinicalDecisionSupport_Tipsheet-.pdf
CMS (Centers for Medicare & Medicaid Services). (2016). Security risk analysis tip sheet: Protect patient health information. Retrieved from https://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/Downloads/2016_SecurityRiskAnalysis.pdf
CMS (Centers for Medicare & Medicaid Services). (2021a). Are you a covered entity? Retrieved from https://www.cms.gov/Regulations-and-Guidance/Administrative-Simplification/HIPAA-ACA/AreYouaCoveredEntity
CMS (Centers for Medicare & Medicaid Services). (2021b). Certified EHR technology. Retrieved from https://www.cms.gov/Regulations-and-Guidance/Legislation/EHRIncentivePrograms/Certification
CMS (Centers for Medicare & Medicaid Services). (2021c). Coding. Retrieved from https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/HospitalAcqCond/Coding
CMS (Centers for Medicare & Medicaid Services). (2021d). MACRA. Retrieved from https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/MACRA-MIPS-and-APMs/MACRA-MIPS-and-APMs
Comprehensive Alcohol Abuse and Alcoholism Prevention, Treatment, and Rehabilitation Act of 1970, 42 U.S.C. 4582 (1970).
Conn, J. (2016). Hospital pays hackers $17,000 to unlock EHRs frozen in “ransomware” attack. Retrieved from http://www.modernhealthcare.com/article/20160217/NEWS/160219920
Craswell, A., Bennett, K., Dalgliesh, B., Morris-Smith, B., Hanson, J., Flynn, T., & Wallis, M. (2020). The impact of automated medicine dispensing units on nursing workflow: A cross-sectional study. International Journal of Nursing Studies, 111. https://doi.org/10.1016/j.ijnurstu.2020.103773
Custer, W. S. (2020). Telehealth. Journal of Financial Service Professionals, 74(5), 34–36.
Diaz, N. (2023). HHS releases AI transparency rule. Retrieved from https://www.beckershospitalreview.com/healthcare-information-technology/hhs-releases-ai-rules-for-2024.html
Denis, J. L., & Forest, P. G. (2012). Real reform begins within: An organizational approach to health care reform. Journal of Health Politics, Policy & Law, 37(4), 633–645. https://doi.org/10.1215/03616878-1597457
Digital Health. (2021). US institute publishes core capabilities for EHRs. Retrieved from https://www.digitalhealth.net/2003/08/us-institute-publishes-core-capabilities-for-ehrs/
Doraiswamy, S., Jithesh, A., Mamtani, R., Abraham, A., & Cheema, S. (2021). Telehealth use in geriatrics care during the COVID-19 pandemic- A scoping review and evidence synthesis. International Journal of Environmental Research and Public Health, 18(4). https://doi.org/10.3390/ijerph18041755
Drug Abuse Prevention, Treatment, and Rehabilitation Act of 1972. Act 63 of 1972 § 1690.102 (1972).
Dupont, H., Payen, J.-F., Radjou, A., Choukroun, G., Charpentier, J., Crova, P., Schwebel, C., Lanceleur, A., Slama, M., Luyt, C.-E., Boutonnet, M., Pessey, F., Tran-Van, D., Patrigeon, R.-G., Salah, A. B., Cordier, P.-Y., Lyochon, A., Boussen, S., Cungi, P.-J., … Goutorbe, P. (2019). Rapid sequence induction traceability in an ICU dedicated patient data management system: A multicentric retrospective study. Journal of Critical Care, 54, 292–297. https://doi.org/10.1016/j.jcrc.2019.08.021
Evident. (2023). Why you should create a standardization plan for your EHRs. Retrieved from https://www.evident.com/resources/blogs/why-you-should-create-a-standardization-plan-for-your-ehrs/
Excite Health Partners. (2012). ARRA, the HITECH Act, and Meaningful Use – an overview. Retrieved from https://excitehealthpartners.com/insight-learning/arra-the-hitech-act-and-meaningful-use-an-overview/
Fakroon, M., Gebali, F., & Mamun, M.S. (2020). Multifactor authentication scheme using physically unclonable functions. Internet Things, 13, 100343. DOI:10.1016/j.iot.2020.100343
Fernandez, M. (2018). Artificial Intelligence in healthcare takes precision medicine to the next level. Retrieved from https://www.frost.com/news/press-releases/artificial-intelligence-healthcare-takes-precision-medicine-next-level/
Gao, Y., Nocon, R. S., Gunter, K. E., Sharma, R., Ngo-Metzger, Q., Casalino, L. P., & Chin, M. H. (2016). Characteristics associated with patient-centered medical home capability in health centers: A cross-sectional analysis. Journal of General Internal Medicine, 31(9), 1041. https://doi.org/10.1007/s11606-016-3729-8
Garrett, P. & Seidman, J. (2011). EMR vs EHR – What is the difference? Retrieved from https://www.healthit.gov/buzz-blog/electronic-health-and-medical-records/emr-vs-ehr-difference
Goodenough, S. (2009). Semantic interoperability, e-health and Australian health statistics. Health Information Management Journal, 38(2), 41–45. https://doi.org/10.1177/183335830903800206
Graham, F., Boland, P., Wallace, S., Taylor, W. J., Jones, B., Maggo, J., & Grainger, R. (2021). Social and technical readiness for a telehealth assessment service for adults with complex wheelchair and seating needs: A national survey of stakeholders. New Zealand Journal of Physiotherapy, 49(1), 31–39. https://doi.org/10.15619/nzjp/49.1.05
Hanson, A. & Haddad, L. M. (2021). Nursing rights of medication administration. StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing. Retrieved from https://www.ncbi.nlm.nih.gov/books/NBK560654/
HealthCare. (n.d.). Affordable Care Act (ACA). Retrieved from https://www.healthcare.gov/glossary/affordable-care-act/
HealthIT. (2013). How does the HITECH Act address barriers to information exchange? Retrieved from https://www.healthit.gov/faq/how-does-hitech-act-address-barriers-information-exchange
HealthIT. (2015). Guide to privacy and security of electronic health information. Retrieved from https://www.healthit.gov/sites/default/files/pdf/privacy/privacy-and-security-guide.pdf
HealthIT. (2017). Permitted uses and disclosures: Exchange for health oversight activities 45 Code of Federal Regulations (CFR) 164.512(d). Retrieved from https://www.healthit.gov/sites/default/files/phi_permitted_uses_and_disclosures_fact_sheet_012017.pdf
HealthIT. (2019). Health IT standards. Retrieved from https://www.healthit.gov/topic/standards-technology/health-it-standards
HealthIT. (2021a). Health IT legislation. Retrieved from https://www.healthit.gov/topic/laws-regulation-and-policy/health-it-legislation
HealthIT. (2021b). STAR HIE program. Retrieved from https://www.healthit.gov/topic/star-hie-program
HealthIT. (2021c). What are the different types of health information exchange? Retrieved from https://www.healthit.gov/faq/what-are-different-types-health-information-exchange
HealthIT. (2024a). Trusted Exchange Framework and Common Agreement (TEFCA). Retrieved from https://www.healthit.gov/topic/interoperability/policy/trusted-exchange-framework-and-common-agreement-tefca
HealthIT. (2024b). Health Data, Technology, and Interoperability: Certification Program Updates, Algorithm Transparency, and Information Sharing (HTI-1) Final Rule. Retrieved from https://www.healthit.gov/topic/laws-regulation-and-policy/health-data-technology-and-interoperability-certification-program
HL7 (Health Level Seven). (2021). Introduction to HL7 standards. Retrieved from https://www.hl7.org/implement/standards/index.cfm?ref=nav
Health Information Technology Oversight Council (HITOC). (2021). Health information technology oversight council. Retrieved from https://www.oregon.gov/oha/HPA/OHIT-HITOC/Pages/index.aspx
HealthyPeople. (2022). Social determinants of health. Retrieved from https://wayback.archive-it.org/5774/20220413203948/https://www.healthypeople.gov/2020/topics-objectives/topic/social-determinants-of-health
Hertzog, T. (2010). Dissecting physician resistance to CPOE. Retrieved from http://healthsystemcio.com/2010/06/23/dissecting-physician-resistance-to-cpoe/
HIPAA Journal. (2022). What is the HITECH Act? Retrieved from https://www.hipaajournal.com/what-is-the-hitech-act/
HHS (Health and Human Services). (1994). Confidentiality of Patient Records for Alcohol and Other Drug Treatment. Retrieved from http://adaiclearinghouse.org/downloads/tap-13-confidentiality-of-patient-records-for-alcohol-and-other-drug-treatment-103.pdf
HHS. (2017). HITECH Act enforcement interim final rule. Retrieved from https://www.hhs.gov/hipaa/for-professionals/special-topics/hitech-act-enforcement-interim-final-rule/index.html
HHS. (2019). Health IT privacy and security resources for providers. Retrieved from https://www.healthit.gov/topic/privacy-security-and-hipaa/health-it-privacy-and-security-resources-providers
HHS. (2022). What is telehealth? Retrieved from https://telehealth.hhs.gov/patients/understanding-telehealth/
HIMSS (Health Information Management Systems Society). (2021). Interoperability in healthcare. Retrieved from https://www.himss.org/resources/interoperability-healthcare
IBM. (2020). Robotic process automation. Retrieved from https://www.ibm.com/cloud/learn/rpa
IHI (Institute for Healthcare Improvement). (2015). 10 new rules to accelerate healthcare redesign. Retrieved from https://www.ihi.org/Engage/collaboratives/LeadershipAlliance/Documents/LoehrerFeeleyBerwick_10NewRulesAccelerateHCRedesign_HCExecNov15.pdf
IOM (Institute of Medicine). (1999). To err is human: Building a safer health system, Institute of Medicine (U.S.) Committee on Quality of Health Care in America, Washington, DC: National Academy Press.
IOM (Institute of Medicine). (2001). Crossing the quality chasm: A new health system for the 21st century, Institute of Medicine (U.S.) Committee on Quality of Health Care in America, Washington, DC: National Academy Press.
Institute of Medicine (US) Committee on Data Standards for Patient Safety. Key Capabilities of an Electronic Health Record System: Letter Report. Washington (DC): National Academies Press (US); 2003. KEY CAPABILITIES OF AN ELECTRONIC HEALTH RECORD SYSTEM Letter Report. Available from: https://www.ncbi.nlm.nih.gov/books/NBK221800/
IOM report: patient safety–achieving a new standard for care. (2005). Aspden P, Corrigan JM, Wolcott J, Erickson SM, editors. Washington (DC): National Academies Press (US); 2004. PMID: 25009854. https://doi.org/10.1197/j.aem.2005.07.010
Juneja, M. (2022). What are the big ethical challenges for AI in healthcare? Retrieved from https://www.hallandpartners.com/thinking/transform/big-ethical-challenges-for-ai-in-healthcare
Kelly, J. T., Campbell, K. L., Gong, E., & Scuffham, P. (2020). The Internet of Things: Impact and implications for health care delivery. Journal of medical Internet research, 22(11), e20135. https://doi.org/10.2196/20135
Kim, M., Yu, S., Lee J, Park Y, Park Y. (2020). Design of Secure Protocol for Cloud-Assisted Electronic Health Record System Using Blockchain. Sensors (Basel), 20(10):2913. doi: 10.3390/s20102913.
Kloss, L. L. (2019). Exercising personal health information access rights: A proactive primer on enforcing health information rights and accessing personal medical data. Generations, 43(4), 38–45.https://www-jstor-org.csuglobal.idm.oclc.org/stable/26908291
Legaz-García, M. del C., Martínez-Costa, C., Menárguez-Tortosa, M., & Fernández-Breis, J. T. (2016). A semantic web based framework for the interoperability and exploitation of clinical models and EHR data. Knowledge-Based Systems, 105, 175–189. https://doi.org/10.1016/j.knosys.2016.05.016
Lewis, M. (2021). States acting to expand telehealth. APTA Magazine, 13(1), 14–17.
Lieneck, C., Weaver, E., & Maryon, T. (2021). Outpatient telehealth Implementation in the United States during the COVID-19 global pandemic: A systematic review. Medicina (Kaunas, Lithuania), 57(5). https://doi.org/10.3390/medicina57050462
Maheu. (2021). Telemedicine across state lines post-pandemic. Retrieved from https://telehealth.org/telemedicine-across-state-lines/
Menachemi, N., Rahurkar, S., Harle, C.A., & Vest, J.R. (2018). The benefits of health information exchange: an updated systematic review. J Am Med Inform Assoc. 25(9):1259-1265. doi: 10.1093/jamia/ocy035. PMID: 29718258
NASA. (2020). A brief history of NASA’s contributions to telemedicine. Retrieved from https://www.nasa.gov/content/a-brief-history-of-nasa-s-contributions-to-telemedicine/
Nicosia, F. M., Kaul, B., Totten, A. M., Silvestrini, M. C., Williams, K., Whooley, M. A., & Sarmiento, K. F. (2021). Leveraging telehealth to improve access to care: a qualitative evaluation of veterans’ experience with the VA TeleSleep program. BMC Health Services Research, 21(1), 77. https://doi.org/10.1186/s12913-021-06080-5
NIST Releases Draft Security Feature Recommendations for IoT Devices. National Institute of Standards and Technology. 2019. [2020-02-02]. https://www.nist.gov/news-events/news/2019/08/nist-releases-draft-security-feature-recommendations-iot-devices
NLM. (2021). SNOMED CT. Retrieved from https://www.nlm.nih.gov/healthit/snomedct/index.html
Oh, J-W., Kang, J-K., & Park, J-Y. (2019). A Study of Smart Healthcare Service Model Based on Cloud Platform: Focus on small and Medium sized Hospitals. Medico-Legal Update, 19(2), 434–440. https://doi.org/10.5958/0974-1283.2019.00216.0
Oo, H. M., Htun, Y. M., Win, T. T., Han, Z. M., Zaw, T., & Tun, K. M. (2021). Information and communication technology literacy, knowledge and readiness for electronic medical record system adoption among health professionals in a tertiary hospital, Myanmar: A cross-sectional study. PloS One, 16(7), e0253691. https://doi.org/10.1371/journal.pone.0253691
Project Management Institute. (2020). 5 phases of project management life cycle you need to know. Retrieved from https://project-management.com/project-management-phases/
Purnell, S., & Zheng, F. (2021). Safety of surgical telehealth in the outpatient and inpatient setting. The Surgical Clinics of North America, 101(1), 109–119. https://doi.org/10.1016/j.suc.2020.09.003
Rangachari, P., Mushiana, S. S., & Herbert, K. (2021). A narrative review of factors historically influencing telehealth use across six medical specialties in the United States. International Journal of Environmental Research and Public Health, 18(9). https://doi.org/10.3390/ijerph18094995
Ratia, M., Myllärniemi, J., & Helander, N. (2018). Robotic Process Automation – Creating Value by Digitalizing Work in the Private Healthcare? Proceedings of the 22nd International Academic Mindtrek Conference, 222–227. https://doi.org/10.1145/3275116.3275129
Ristevski, B., & Chen, M. (2018). Big Data Analytics in Medicine and Healthcare. Journal of integrative bioinformatics, 15(3), 20170030. https://doi.org/10.1515/jib-2017-0030
Sachdeva, S., & Bhalla, S. (2012). Semantic interoperability in standardized electronic health record databases. Journal of Data and Information Quality (JDIQ), 3(1), 1–37. https://doi.org/10.1145/2166788.2166789
Shah, N., & Jani, Y. (2020). Implementation of smart infusion pumps: A scoping review and case study discussion of the evidence of the role of the pharmacist. Pharmacy (Basel, Switzerland), 8(4). https://doi.org/10.3390/pharmacy8040239
Softermii. (2022). Video conferencing security: How to eliminate cyber threats for your video conferencing system. Retrieved from https://www.softermii.com/blog/how-to-eliminate-cyber-threats-for-your-video-conferencing-and-chatting-system
Standish Group. (2015). Chaos Report. Retrieved from https://www.infoq.com/articles/standish-chaos-2015
The National Academies Press. (1991). Medicare: New directions in quality assurance proceedings. Retrieved from https://www.nap.edu/read/1768/chapter/4
Thede, L. Q. & Sewell, J. P. (2012). Computer development and health care information systems 1950 to present. Retried from http://dlthede.net/Informatics/Chap01IntroNI/healthcare_computers.html
Tompkins McMahon, J. 2017. “Improving medication administration safety in the clinical environment.” MEDSURG Nursing 26 (6): 374–409. https://search.ebscohost.com/login.aspx?direct=true&db=c8h&AN=126865007&site=eds-live.
Truran, D., Saad, P., Ming Zhang, & Innes, K. (2010). SNOMED CT and its place in health information management practice. Health Information Management Journal, 39(2), 37–39. https://doi.org/10.1177/183335831003900206
Ullah, F., Habib, M. A., Farhan, M., Khalid, S., Durrani, M. Y., & Jabbar, S. (2017). Semantic interoperability for big-data in heterogeneous IoT infrastructure for healthcare. Sustainable Cities and Society, 34, 90–96. https://doi.org/10.1016/j.scs.2017.06.010
Walkweltech. (2019). HIPAA and blockchain. Retrieved from https://www.walkweltech.com/blog/hipaa-and-blockchain/
Welkin Health. (2020). The ultimate guide to remote patient monitoring devices. Retrieved from https://welkinhealth.com/remote-patient-monitoring-devices/#
Westwood, A. R. (2021). Telehealth and maternity: Has the onset of the pandemic changed the way we utilise telemedicine forever? British Journal of Midwifery, 29(6), 352–355. https://doi.org/10.12968/bjom.2021.29.6.352
Willett, D. L., Kannan, V., Chu, L., Buchanan, J. R., Velasco, F. T., Clark, J. D., Fish, J. S., Ortuzar, A. R., Youngblood, J. E., Bhat, D. G., & Basit, M. A. (2018). SNOMED CT concept hierarchies for sharing definitions of clinical conditions using electronic health record data. Applied Clinical Informatics, 9(3), 667–682. https://doi.org/10.1055/s-0038-1668090
WorldVistA. (2004). VistA history. Retrieved from http://worldvista.sourceforge.net/vista/history/
Xu, R., Chen, Y., Chen, G., & Blasch, E. (2022). SAUSA: Securing Access, Usage, and Storage of 3D Point CloudData by a Blockchain-Based Authentication Network. Future Internet, 14(12), 354. https://doi.org/10.3390/fi14120354
Zhang, C., Issa, H., Rozario, A., & Soegaard, J. S. (2023). Robotic Process Automation (RPA) Implementation Case Studies in Accounting: A Beginning to End Perspective. Accounting Horizons, 37(1), 193–217. https://doi.org/10.2308/HORIZONS-2021-084
Zimmerman, M., Benjamin, I., Tirpak, J. W., & D’Avanzato, C. (2021). Patient satisfaction with partial hospital telehealth treatment during the COVID-19 pandemic: Comparison to in-person treatment. Psychiatry Research, 301, 113966. https://doi.org/10.1016/j.psychres.2021.113966